The Impact of Microvascular Inflammation (MVI) in Kidney Transplant Biopsies (KTxBx) Is Independent of Time Post-Transplant.
1Dept. of Medicine, University of Alabama at Birmingham, Birmingham, AL
2Dept of Lab Medicine &
Pathology, Mayo Clinic College of Medicine, Rochester, MN
3Division of Biostatistics, U. Minnesota School of Public Health, Minneapolis, MN.
Meeting: 2016 American Transplant Congress
Abstract number: D21
Keywords: Alloantibodies, Graft survival, Histology, Rejection
Session Information
Session Name: Poster Session D: Antibody Mediated Rejection: Session #2
Session Type: Poster Session
Date: Tuesday, June 14, 2016
Session Time: 6:00pm-7:00pm
 Presentation Time: 6:00pm-7:00pm
Presentation Time: 6:00pm-7:00pm
Location: Halls C&D
Detection of MVI in a KTxBx, often associated with antibody mediated rejection, is associated with a poor prognosis for kidney graft survival. However most information about the significance of MVI derives from studies of biopsies taken early within the post-transplant period.
The objective of this study was to compare the impact of MVI in KTxBx as a function of biopsy time since transplant (Tp) among 478 patients biopsied later (≥ 3 months) after Tp due to new onset kidney graft dysfunction (25% increase in Scr or new onset proteinuria) enrolled in the two Deterioration of Kidney Allograft Function (DeKAF) Study cohorts (cross sectional (CSC): 229 patients; prospective (PC) 249 patients). Biopsies showing other causes of graft dysfunction (recurrent glomerulonephritis, BK nephropathy, and transplant glomerulopathy) were excluded. MVI was diagnosed by any Banff ptc or g score > 0. Time from Tp to biopsy in the two cohorts differed substantially (median ⦥ for PC patients: 12.5 [3.0 – 55.4]; for CSC patients: 76.0 [7.4 – 313.1 months). We assessed impact of MVI across time from Tp to biopsy by comparing within cohort the hazard ratio (HR) for death censored graft failure between biopsies obtained before or after the median biopsy times post Tp.
MVI was associated with a 2.8 fold increased HR for graft failure (95% Confidence Interval (95% CI): 2.0 – 4.0; p < 0.0001). The baseline HR for the CSC was slightly but not significantly greater than for the PC (HR [95% CI]: 1.23 [0.88 – 1.72], p = 0.22). The hazard ratio for MVI did not differ within cohort between shorter and longer times from Tp to KTxBx (all p-values > 0.35) or between cohort. Figure 1 shows Kaplan-Meier survival curves for grafts with MVI in this analysis.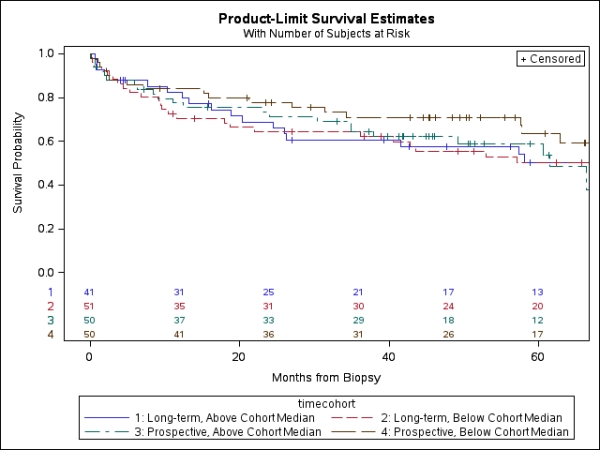
In sum, the impact of MVI on graft survival following KtxBx for cause ≥ 3 months post Tp did not differ between shorter or longer periods of time between Tp and biopsy.
CITATION INFORMATION: Gaston R, Grande J, Leduc R, The DeKAF Study Group The Impact of Microvascular Inflammation (MVI) in Kidney Transplant Biopsies (KTxBx) Is Independent of Time Post-Transplant. Am J Transplant. 2016;16 (suppl 3).
To cite this abstract in AMA style:
Gaston R, Grande J, Leduc R, Group TheDeKAFStudy. The Impact of Microvascular Inflammation (MVI) in Kidney Transplant Biopsies (KTxBx) Is Independent of Time Post-Transplant. [abstract]. Am J Transplant. 2016; 16 (suppl 3). https://atcmeetingabstracts.com/abstract/the-impact-of-microvascular-inflammation-mvi-in-kidney-transplant-biopsies-ktxbx-is-independent-of-time-post-transplant/. Accessed February 21, 2026.« Back to 2016 American Transplant Congress
