The Correlation of Hepatic and Systemic Hemodynamics During Liver Transplantation: Quantification of Hepatic Resistance as an Actual Value.
A.-C. Feng, T.-W. Chen, H.-L. Fan, J.-C. Yu, C.-B. Hsieh.
Surgery, Tri-Service General Hospital, National Defense Medical Center, Taipei, Taiwan.
Meeting: 2016 American Transplant Congress
Abstract number: C212
Keywords: Liver metabolism, Liver transplantation, Post-operative complications
Session Information
Session Name: Poster Session C: Liver Transplantation Complications and Other Considerations
Session Type: Poster Session
Date: Monday, June 13, 2016
Session Time: 6:00pm-7:00pm
 Presentation Time: 6:00pm-7:00pm
Presentation Time: 6:00pm-7:00pm
Location: Halls C&D
Purpose
The correlation between portal vein pressure (PVP) and flow (PVF) has not been established, and there is still lack of consensus about the optimal hemodynamics during liver transplantation (LT). We aimed to establish this hemodynamic correlation during LT by applying the hepatokinetic power hypothesis, based on the law of energy conservation and hydrodynamics. The hepatokinetic power equation is derived from a series of mathematical substitution, and the equation is presented as:
HKPG=PVP[times]PVF+MAP[times]HAF–CVP[times](PVF+HAF)
HKPG, hepatokinetic power gradient; MAP, mean arterial pressure; HAF, hepatic artery flow; CVP, central venous pressure 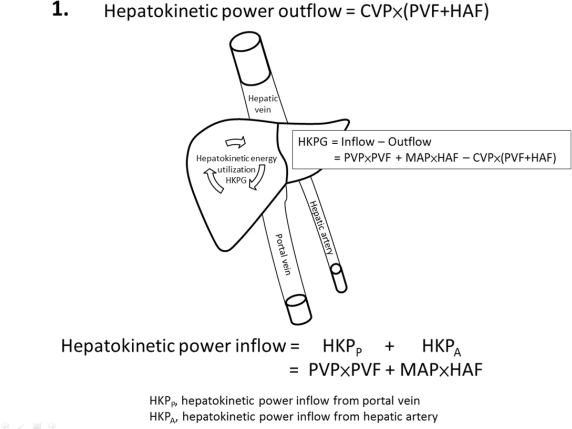
Materials and Methods
A total of 103 adult liver transplant recipients were enrolled in this study from September 2012-December 2014. Systemic and hepatic hemodynamics were assessed intra-operatively to calculate the hepatokinetic power status. Severe surgical complications (Clavien-Dindo grade≥III) were recorded as the main outcome measure, and potential covariates were evaluated including recipient, donor, donor-recipient match, surgery-related factors, conventional hemodynamics, and the intra-operative hepatokinetic power profile.
Results
In multivariate analysis, hepatokinetic power gradient>4260 mLmmHg min-1100 g graft weight-1 (P=0.001), 2.2<ratio of hepatokinetic power from the portal vein to the hepatic artery≤8.7 (P=0.012), and hepatic resistance of partial grafts≤0.006 or >0.015 min mmHg mL-1 (P=0.012) were associated with a higher risk. None of the conventional hemodynamic parameters, such as PVP, PVF and hepatic venous pressure gradient, entered into this regression model (c-statistic=0.916) when competing with hepatokinetic power indexes.
Conclusion
The hepatokinetic power hypothesis clarifies the correlation of systemic and hepatic hemodynamics in a simple, rational manner. The hepatic resistance, derived from the hepatokinetic power equation, can be quantified and has an effect on the incidence of severe surgical complications. This finding offers a new objective clinical approach to evaluate graft quality during transplantation.
CITATION INFORMATION: Feng A.-C, Chen T.-W, Fan H.-L, Yu J.-C, Hsieh C.-B. The Correlation of Hepatic and Systemic Hemodynamics During Liver Transplantation: Quantification of Hepatic Resistance as an Actual Value. Am J Transplant. 2016;16 (suppl 3).
To cite this abstract in AMA style:
Feng A-C, Chen T-W, Fan H-L, Yu J-C, Hsieh C-B. The Correlation of Hepatic and Systemic Hemodynamics During Liver Transplantation: Quantification of Hepatic Resistance as an Actual Value. [abstract]. Am J Transplant. 2016; 16 (suppl 3). https://atcmeetingabstracts.com/abstract/the-correlation-of-hepatic-and-systemic-hemodynamics-during-liver-transplantation-quantification-of-hepatic-resistance-as-an-actual-value/. Accessed January 7, 2026.« Back to 2016 American Transplant Congress
