Susceptibility Patterns of Pre-Transplant Pseudomonas and Post-Lung Transplant Outcomes in Patients with Cystic Fibrosis.
1Ohio State University, Columbus, OH
2University of Washington, Seattle, WA
3University of Pittsburgh, Pittsburgh, PA
4Stanford University, Stanford, CA
5University of Iowa, Iowa City, IA
6Washington University St. Louis, St. Louis, MO
7Massachusetts General Hospital, Boston, MA
8Vanderbilt University, Nashville, TN
9University of California San Diego, San Diego, CA
10University of Alabama, Birmingham, AB
11Ochsner Clinic Foundation, New Orleans, LA
12University of Alberta, Edmonton, AB, Canada
13Nationwide Children's Hospital, Columbus, OH
14University of North Carolina, Chapel Hill, NC.
Meeting: 2016 American Transplant Congress
Abstract number: B283
Keywords: Lung infection, Lung transplantation, Mortality, Rejection
Session Information
Session Name: Poster Session B: Lung Transplantation Posters
Session Type: Poster Session
Date: Sunday, June 12, 2016
Session Time: 6:00pm-7:00pm
 Presentation Time: 6:00pm-7:00pm
Presentation Time: 6:00pm-7:00pm
Location: Halls C&D
Background: The impact of pre-lung transplant (LT) pan-drug-resistant Pseudomonas aeruginosa (PDR PsA) colonization on post-LT mortality and bronchiolitis obliterans syndrome (BOS) rates in cystic fibrosis (CF) LT recipients (LTR) is unknown.
Methods: Retrospective, multicenter study from 1/1/2010 to 12/31/2011 of CF LTR with PsA airway colonization within 6 months of LT with 3 years of follow-up post-LT.
Results: 14 centers enrolled 99 LTR (median lung allocation score 40 [IQR 37-51]). 52/99 (53%) LTR had pre-LT PDR PsA. LTR with PDR PsA were older (median age 29 [IQR 25-36] vs 24 years [IQR 19-29], p<0.01), received more peri-LT antibiotics (median 4 [IQR 3-5] vs 3 [IQR 3-4], p<0.01), were more likely to receive induction therapy (88% vs 70%, p=0.02), and had a longer post-LT length of stay (LOS, mean 29 vs 19 days, p<0.05). Rates of BOS (19% vs 36%, [p=0.07]), 3-year mortality (17% vs 30%, [p=0.16]) and time from LT to BOS or death were similar among LTR with vs without PDR PsA. 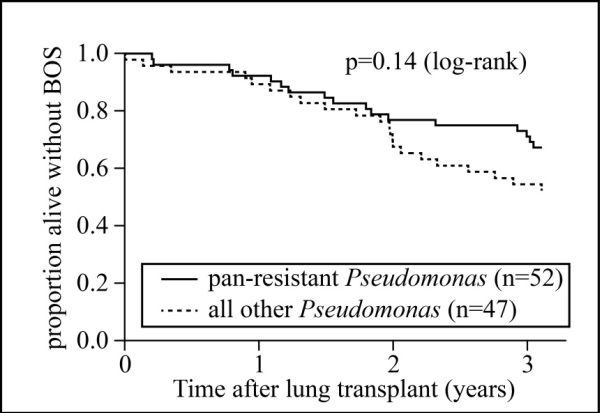
Conclusions: While PDR PsA colonization is associated with longer post-LT LOS in CF LTR, rates of post-LT BOS and mortality were similar in patients with PDR vs other PsA.
CITATION INFORMATION: Pouch S, Lease E, Bogdanovich T, Ho D, Miller R, Estabrook M, Babu T, Kotton C, Shaver C, Thomas L, Aslam S, McCarty T, Garcia-Diaz J, Doucette K, Kirkby S, van Duin D. Susceptibility Patterns of Pre-Transplant Pseudomonas and Post-Lung Transplant Outcomes in Patients with Cystic Fibrosis. Am J Transplant. 2016;16 (suppl 3).
To cite this abstract in AMA style:
Pouch S, Lease E, Bogdanovich T, Ho D, Miller R, Estabrook M, Babu T, Kotton C, Shaver C, Thomas L, Aslam S, McCarty T, Garcia-Diaz J, Doucette K, Kirkby S, Duin Dvan. Susceptibility Patterns of Pre-Transplant Pseudomonas and Post-Lung Transplant Outcomes in Patients with Cystic Fibrosis. [abstract]. Am J Transplant. 2016; 16 (suppl 3). https://atcmeetingabstracts.com/abstract/susceptibility-patterns-of-pre-transplant-pseudomonas-and-post-lung-transplant-outcomes-in-patients-with-cystic-fibrosis/. Accessed February 21, 2026.« Back to 2016 American Transplant Congress
