Morbidity and Mortality of Early Post-Operative Acute Kidney Injury in Cardiothoracic Transplant Recipients.
Tampa General Hospital, Tampa, FL.
Meeting: 2016 American Transplant Congress
Abstract number: B151
Keywords: Heart transplant patients, Lung transplantation, Renal injury
Session Information
Session Name: Poster Session B: Hearts and VADs in Depth - The Force Awakens
Session Type: Poster Session
Date: Sunday, June 12, 2016
Session Time: 6:00pm-7:00pm
 Presentation Time: 6:00pm-7:00pm
Presentation Time: 6:00pm-7:00pm
Location: Halls C&D
Purpose: Early acute kidney injury (AKI) in cardiothoracic transplant recipients (CTTR) has not been well described; renal injury defined by the RIFLE criteria has been associated with increased morbidity and mortality in non-transplant populations. We sought to define the incidence, risk factors, and outcomes associated with early AKI after CTTR.
Methods: An analysis of all CTTR at a single center from 10/2011-09/2014 was conducted; re-transplant and multi-organ recipients were excluded. Renal Risk (SCr 1.5x baseline), Injury (SCr 2x baseline), Failure (SCr 3x baseline), Loss (renal replacement therapy [RRT] >4 weeks), and End-Stage disease (RRT >3 months) (RIFLE) criteria were applied to determine the extent, if any, of AKI 72 hours post-operatively. Risk factors for and 1 year outcomes of AKI were assessed.
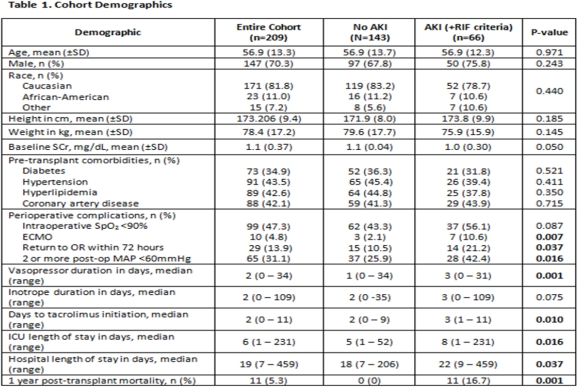
Results: 209 CTTR (heart transplant: n=125, lung transplant: n=84) were included (Table 1). Sixty-six (31.6%) CTTR met criteria for risk, 26 (12.4%) for injury, and 5 (2.4%) for failure. Seven patients with AKI progressed to end-stage disease, all requiring RRT at 1 year after transplant. Mortality at 1 year post-transplant was significantly higher in those who experienced AKI (+RIF) compared to those without AKI (11 vs. 0%, p<0.001). Both ICU and hospital length of stay were significantly longer in the AKI cohort. The impact of patient and perioperative complications on development of AKI was assessed (Table 1). Significant perioperative complications and longer duration of vasopressor support were associated with AKI and likely represents a more acutely ill cohort. Age, sex, race, and pre-transplant comorbidities were not associated with development of AKI. As expected, the development of AKI was associated with delayed initiation of tacrolimus.
Conclusions: Early post-operative AKI is associated with significant morbidity and mortality in CTTR. There were no identifiable pre-transplant risk factors for AKI development; ischemic risk factors in the perioperative period appear to be the major contributor to renal injury.
CITATION INFORMATION: Casale J, Logan A, Doligalski C. Morbidity and Mortality of Early Post-Operative Acute Kidney Injury in Cardiothoracic Transplant Recipients. Am J Transplant. 2016;16 (suppl 3).
To cite this abstract in AMA style:
Casale J, Logan A, Doligalski C. Morbidity and Mortality of Early Post-Operative Acute Kidney Injury in Cardiothoracic Transplant Recipients. [abstract]. Am J Transplant. 2016; 16 (suppl 3). https://atcmeetingabstracts.com/abstract/morbidity-and-mortality-of-early-post-operative-acute-kidney-injury-in-cardiothoracic-transplant-recipients/. Accessed February 23, 2026.« Back to 2016 American Transplant Congress
