Waitlist Outcomes of Patients Re-Listed Following Failed Donation After Cardiac Death (DCD) Liver Transplant.
Transplant, Mayo Clinic Florida, Jacksonville, FL
Meeting: 2017 American Transplant Congress
Abstract number: C176
Keywords: Donors, Graft failure, non-heart-beating, Waiting lists
Session Information
Session Name: Poster Session C: Organ Allocation, Meld Score, Organ Utilization, and Transplant Outcomes
Session Type: Poster Session
Date: Monday, May 1, 2017
Session Time: 6:00pm-7:00pm
 Presentation Time: 6:00pm-7:00pm
Presentation Time: 6:00pm-7:00pm
Location: Hall D1
Introduction: The outcome for patients re-listed after developing ischemic cholangiopathy(IC) or graft failure following liver transplant(LT) from a DCD donor, remains a significant concern. Better understanding of these outcomes are needed as we move forward with policies defining if and how exception points for these patients should be awarded.
Methods: Data on all patients undergoing DCD LT nationally from 2002-2016 were obtained from the UNOS database. Early DCD graft failure(PNF or HAT) was defined as re-listing ≤14days after LT, while late DCD graft failure(IC) was defined as re-listing 14days-3 years after LT.
Results: DCD LT was performed in 3908 cases of which 540(13.8%) patients were re-listed within 3 years of their DCD LT. Median time from DCD LT to relisting was 104 days. At 90 days following re-listing overall mortality rate was 11.5%, transplant rate 34%, delisting for too well 7.4% and still waiting 47%. Patients re-listed for early DCD graft Failure (EDCDGF) had a 90 day mortality of 15.4%, which increased only slightly to 16.1% at 1 year while 25.0% of patients were ultimately de-listed for too-well. For patients who were re-listed for late graft failure(LDCDGF), waitlist mortality rate was: 10.5% at 3 months, 12.4% at 6 months and 14.3% at 1 year. Waitlist mortality for patients re-listed for LDCDGF was significantly higher than mortality/de-listed rate for patients with HCC exception points at 3, 6, 9 and 12 month intervals respectively(p<0.001). In the EDCDGF group 14.3% of patients applied for exception points, all for HAT. In the LDCDGF group 33.1% of patients applied for exceptions. Biologic MELD score for LDCDGF that applied for exceptions was 17.1±8.3 compared to 27.7±7.7 for those that did not. For LDCDGF patients with exceptions, match meld was 28.1±6.7.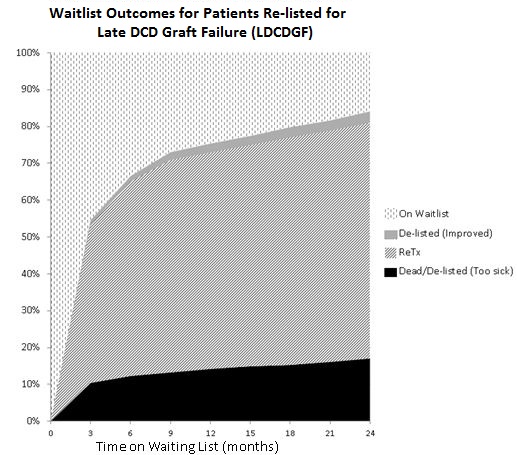 Conclusion: The present study provides a detailed analysis of waitlist outcomes of patients re-listed following failed DCD LT. Waitlist outcomes differed in patients with early DCD graft failure(PNF or HAT) compared to those with late DCD graft failure(IC). These data can provide guidance for determining how and if exception points should be awarded to these patients.
Conclusion: The present study provides a detailed analysis of waitlist outcomes of patients re-listed following failed DCD LT. Waitlist outcomes differed in patients with early DCD graft failure(PNF or HAT) compared to those with late DCD graft failure(IC). These data can provide guidance for determining how and if exception points should be awarded to these patients.
CITATION INFORMATION: Croome K, Lee D, Keaveny A, Taner C. Waitlist Outcomes of Patients Re-Listed Following Failed Donation After Cardiac Death (DCD) Liver Transplant. Am J Transplant. 2017;17 (suppl 3).
To cite this abstract in AMA style:
Croome K, Lee D, Keaveny A, Taner C. Waitlist Outcomes of Patients Re-Listed Following Failed Donation After Cardiac Death (DCD) Liver Transplant. [abstract]. Am J Transplant. 2017; 17 (suppl 3). https://atcmeetingabstracts.com/abstract/waitlist-outcomes-of-patients-re-listed-following-failed-donation-after-cardiac-death-dcd-liver-transplant/. Accessed February 16, 2026.« Back to 2017 American Transplant Congress
