Waitlist Mortality in Children with Biliary Atresia: A Competing Risks Analysis
Vanderbilt University Medical Center, Nashville, TN
Meeting: 2020 American Transplant Congress
Abstract number: 583
Keywords: Allocation, Biliary atresia, Liver transplantation, Waiting lists
Session Information
Session Time: 3:15pm-4:45pm
 Presentation Time: 3:27pm-3:39pm
Presentation Time: 3:27pm-3:39pm
Location: Virtual
*Purpose: Biliary atresia (BA) is the most common indication for liver transplant (LT) in children. The current PELD allocation algorithm does not accurately reflect the degree of illness in BA patients resulting in an increased dependence on exception points. We aimed to describe the cumulative incidence of waitlist death/delisting due to clinical deterioration and to propose a more accurate risk prediction and waitlist prioritization model.
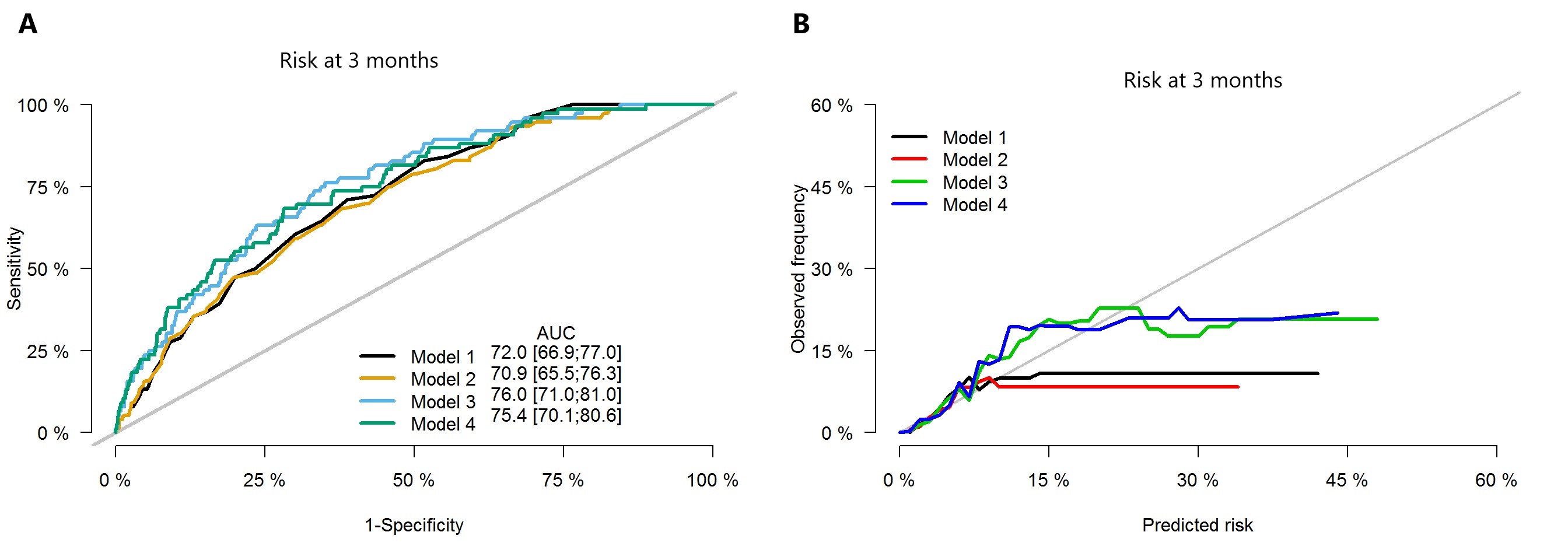
*Methods: All BA patients (<18 years) listed for primary LT (2002-2018) in the UNOS database were identified. Through competing risks analysis (main risk=death/delisting due to clinical deterioration, competing risk=LT), independent risk factors were selected to develop alternative risk prediction models. Nested models were compared with likelihood ratio (LR) tests. Discrimination was evaluated by calculating the area under the curve and calibration by calibration plots.
*Results: 2,714 BA patients with a mean listing age of 1.5 years (range 0-17) were included. 59% were female, the median weight at listing was 7 kg (IQR 5.9-9.5) and the median waitlist time was 81 days (IQR 33-183). The cumulative incidence of waitlist death/delisting due to clinical deterioration was 5.3%. Age, weight, portal vein thrombosis (PVT), ascites, ventilator dependence, laboratory MELD/PELD score, INR, bilirubin, albumin, and Na+ levels at listing (all p≤0.02) were deemed significant on univariate analysis. 4 multivariable models for children <12 years (n=2,065) were constructed: Model 1 (listing PELD), Model 2 (listing PELD, weight), Model 3 (listing PELD, weight, Na+, PVT, ventilator dependence) and Model 4 (listing INR, bilirubin, albumin, weight, Na+, PVT, ventilator dependence). Model 3 had the best performance in terms of both prediction accuracy (AUC=0.75 at 3 months; Figure A) and model calibration (Figure B). The LR test showed significant improvement in Model 3 over Model 1 (p=0.021). No significant differences were detected in terms of model fitting and prediction accuracy between Model 1 and Model 2, as well as between Model 3 and Model 4.
*Conclusions: The current reliance on PELD scores to stratify organ allocation seems inadequate to predict waitlist mortality/delisting due to clinical deterioration. Inclusion of additional risk factors for mortality results in a model to better objectively discriminate between candidates and reduce dependence on subjectively assigned exception scores.
To cite this abstract in AMA style:
Ziogas IA, Ye F, Zhao Z, Matsuoka LK, Montenovo MI, Alexopoulos SP. Waitlist Mortality in Children with Biliary Atresia: A Competing Risks Analysis [abstract]. Am J Transplant. 2020; 20 (suppl 3). https://atcmeetingabstracts.com/abstract/waitlist-mortality-in-children-with-biliary-atresia-a-competing-risks-analysis/. Accessed March 1, 2026.« Back to 2020 American Transplant Congress