Waitlist and Post-Lung Transplant Mortality Vary by Diagnosis for a Given Lung Allocation Score.
JHU, Baltimore
Meeting: 2017 American Transplant Congress
Abstract number: B241
Keywords: Allocation, Lung, Mortality, Outcome
Session Information
Session Name: Poster Session B: Lung Transplantation Poster Session
Session Type: Poster Session
Date: Sunday, April 30, 2017
Session Time: 6:00pm-7:00pm
 Presentation Time: 6:00pm-7:00pm
Presentation Time: 6:00pm-7:00pm
Location: Hall D1
The lung allocation score (LAS) is used to prioritize candidates based on predicted one-year waitlist mortality and post-transplant survival. Lung diagnosis is factored into LAS, as certain diseases demonstrate more rapid decline than others. However, whether a given LAS captures similar risk of mortality across diagnoses is not known but carries important implications for prioritizing a candidate's urgency and post-transplant prognosis.
METHODS: Using SRTR, we studied 10,820 patients listed for lung transplantation between 5/1/2005-7/31/2015. Patients listed at multiple institutions were excluded from waitlist analyses. Cox regression was used to compare mortality by the major diagnoses, classified as: pulmonary hypertension (PH), cystic fibrosis (CF), COPD/emphysema, and idiopathic pulmonary fibrosis (IPF), after adjusting for donor and recipient characteristics as well as transplant procedure type and LAS.
RESULTS: Waitlist and post-transplant mortality varied significantly by diagnosis (Figure; p<0.001). After adjustment, patients with PH had a 4.75 6.48 8.86 times higher risk of waitlist death relative to comparable transplant candidates with COPD/emphysema (Figure; p<0.001). IPF patients had a 24% lower risk of waitlist death compared to COPD/emphysema candidates (aHR = 0.60 0.76 0.95; p<0.05), while CF patients had no significant difference in risk of death compared to COPD/emphysema candidates (p=0.5).
Relative to comparable patients transplanted for COPD/emphysema, for a given LAS, patients with PH had 32% higher risk of post-transplant death (aHR= 1.06 1.32 1.63, p<0.05), while CF patients had 18% lower risk of death (aHR= 0.69 0.82 0.99, p<0.05) and patients with IPF had no statistically significant difference in risk (aHR = 0.87 0.96 1.05, p=0.4).
CONCLUSIONS: Clinicians should be cautious in interpreting LAS, as PH patients have the highest risk of waitlist and post-transplant mortality compared to other diagnoses for a given LAS. Even though LAS factors in diagnosis, policymakers may need to revise the calculation of LAS, as certain diseases may have risk factors that LAS is not weighing accurately.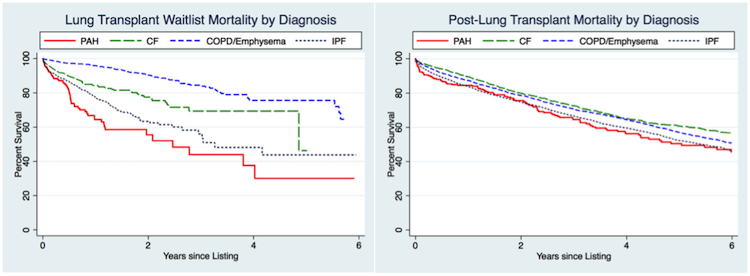
CITATION INFORMATION: Maredia H, Bowring M, Massie A, Oyetunji S, Merlo C, Higgins R, Segev D, Bush E. Waitlist and Post-Lung Transplant Mortality Vary by Diagnosis for a Given Lung Allocation Score. Am J Transplant. 2017;17 (suppl 3).
To cite this abstract in AMA style:
Maredia H, Bowring M, Massie A, Oyetunji S, Merlo C, Higgins R, Segev D, Bush E. Waitlist and Post-Lung Transplant Mortality Vary by Diagnosis for a Given Lung Allocation Score. [abstract]. Am J Transplant. 2017; 17 (suppl 3). https://atcmeetingabstracts.com/abstract/waitlist-and-post-lung-transplant-mortality-vary-by-diagnosis-for-a-given-lung-allocation-score/. Accessed March 7, 2026.« Back to 2017 American Transplant Congress
