Wait Times in Pediatric Heart Transplant Candidates: Impact of Size and Blood Type Following the 2016 Allocation Policy Revision
Department of Cardiology, Boston Children's Hospital, Boston, MA
Meeting: 2020 American Transplant Congress
Abstract number: C-278
Keywords: Allocation, Heart, Pediatric, Waiting lists
Session Information
Session Name: Poster Session C: Heart and VADs: All Topics
Session Type: Poster Session
Date: Saturday, May 30, 2020
Session Time: 3:15pm-4:00pm
 Presentation Time: 3:30pm-4:00pm
Presentation Time: 3:30pm-4:00pm
Location: Virtual
*Purpose: To describe wait times for pediatric heart transplant (HT) candidates following institution of a new allocation system in March 2016.
*Methods: The OPTN database was queried for pediatric HT candidates listed for isolated HT between 7/2016 and 4/2019. Wait times were analyzed by listing status (1A, 1B, 2), blood type, and recipient weight. Candidates were analyzed by days spent at each listing status, classified as transplanted only in their final listing status, and censored in the analysis for any other statuses in which they spent time listed. Wait list outcomes were analyzed using a competing risk analysis and a proportional subdistribution hazards regression model was used to compare associations between predictors and outcomes.
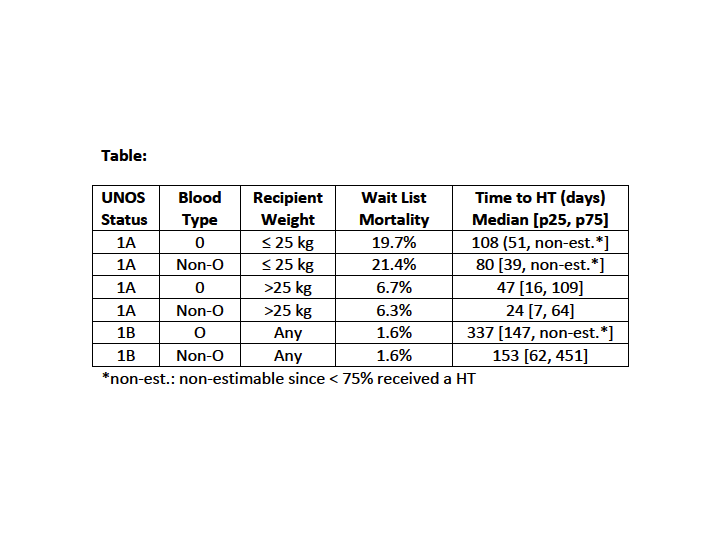
*Results: The study included 1,789 candidates listed for HT under the new allocation system. Of those, 65% underwent HT, 14% died or were removed for clinical deterioration, 8% were removed for other reasons including clinical improvement, and 13% were still waiting at the end of the study period. The majority of children were listed as status 1A at the time of HT (81%), while 16% were listed as status 1B and 2.6% were status 2 at the time of HT. Candidates <25 kg (HR 0.47, CI 0.41-0.54) at listing and blood type O (HR 0.85, CI 0.75-0.96) were less likely to undergo HT. For status 1A candidates, 57% received a HT by 3 months, 72% by 6 months, and 78% by 1 year. Median wait times differed substantially by listing status, blood type and weight (Table). For status 1B candidates, 25% received a HT by 3 months, 42% by 6 months, and 61% by 1 year. Status 2 candidates were unlikely to be transplanted, with only 8% of candidates receiving a HT within 1 year of listing.
*Conclusions: Wait times for pediatric HT candidates are highly variable, with listing status, size, and blood type contributing to wait time and likelihood of HT. Children less than 25 kg, particularly those who are blood type O, experience longer wait times and higher wait list mortality. Advanced heart failure therapies should be selected with these longer wait times in mind.
To cite this abstract in AMA style:
Williams RJ, Lu M, Sleeper LA, Urbach S, Daly KP. Wait Times in Pediatric Heart Transplant Candidates: Impact of Size and Blood Type Following the 2016 Allocation Policy Revision [abstract]. Am J Transplant. 2020; 20 (suppl 3). https://atcmeetingabstracts.com/abstract/wait-times-in-pediatric-heart-transplant-candidates-impact-of-size-and-blood-type-following-the-2016-allocation-policy-revision/. Accessed February 17, 2026.« Back to 2020 American Transplant Congress