Variation in Definition of Death in Donation After Circulatory Death Policies
1University of Michigan Medical School, Ann Arbor, MI, 2Department of Surgery, University of Michigan, Ann Arbor, MI
Meeting: 2022 American Transplant Congress
Abstract number: 1788
Keywords: Donors, non-heart-beating, Ethics, Kidney transplantation, Liver transplantation
Topic: Clinical Science » Organ Inclusive » 68 - Deceased Donor Management and Intervention Research
Session Information
Session Name: Deceased Donor Management and Intervention Research
Session Type: Poster Abstract
Date: Tuesday, June 7, 2022
Session Time: 7:00pm-8:00pm
 Presentation Time: 7:00pm-8:00pm
Presentation Time: 7:00pm-8:00pm
Location: Hynes Halls C & D
*Purpose: Organ transplantation operates through a shared network requiring organizations, hospitals, and individuals to work towards a common goal. However, the policies that govern each organization that affect the shared organ supply may differ. Donation after circulatory death (DCD) protocols are one example of a common policy that has been created and shared, yet variation exists among them. In this study, we set to analyze the language used by DCD policies to define death in DCD donation to investigate variation in practice in a single state.
*Methods: We conducted an analysis of individual hospital DCD policies within the state of Michigan. We examined the policies for their differences and similarities across protocols. We hypothesized there would be institutional variance in the definition of death, the provider who can declare death, and the maximum wait time for the donor to expire after extubation until organ recovery is no longer pursued.
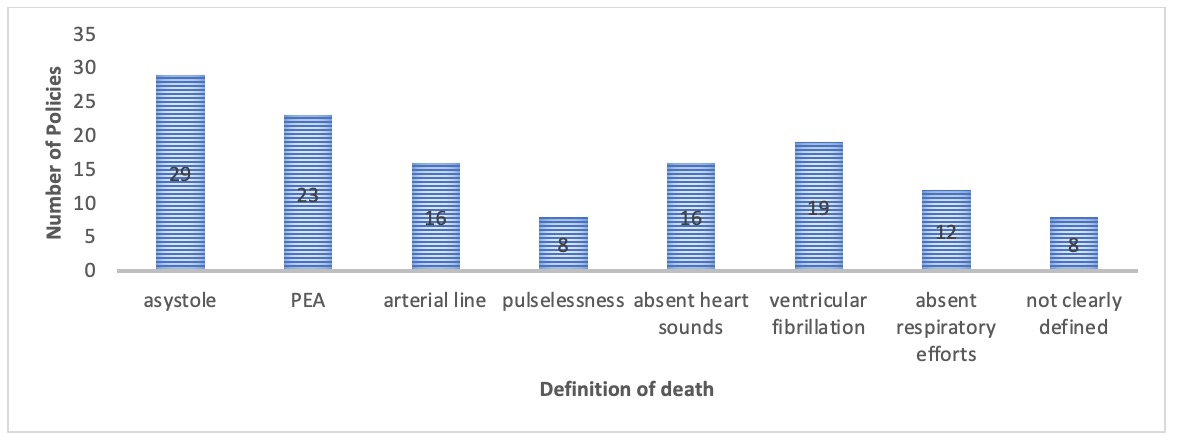
*Results: Fifty policies were included in our analysis. Most hospitals (94% n=47) required a physician to declare death in DCD and this physician must be separate from the recovering surgical team. Twenty-two policies (44%) note that physician designees, which may include residents, RNs and other team members, are permitted to declare death. The minutes to expire ranged from 60 to 120 minutes, with the majority of (44%, n=22) hospitals setting the maximum time to expire at 90 minutes. There was significant variation in how each hospital defined death, however, consistent themes were asystole, pulseless electrical activity (PEA) and ventricular fibrillation. The most common definition included asystole. Eight hospitals did not clearly define the declaration of death.
*Conclusions: National recommendations define death in DCD recoveries as PEA, however, there is wide variation in the interpretation of these recommendations. Guidance from varied DCD policies to wait for asystole may cause delays in organ recovery. The difference between PEA and asystole may result in time lost and organs becoming nonviable. Standard policies and increased education to physicians and designees that declare death in DCD recoveries are vital as the surgical team cannot communicate with the declaring providers during the DCD recovery. Lack of standardization may result in less trust among institutions that recover and receive organs, more room for error for traveling transplant surgeons in recovery operations, and inconsistencies in DCD data.
To cite this abstract in AMA style:
Cassidy D, Englesbe MJ, Valbuena VS. Variation in Definition of Death in Donation After Circulatory Death Policies [abstract]. Am J Transplant. 2022; 22 (suppl 3). https://atcmeetingabstracts.com/abstract/variation-in-definition-of-death-in-donation-after-circulatory-death-policies/. Accessed February 24, 2026.« Back to 2022 American Transplant Congress