Variation in Adult Living Donor Liver Transplantation in the United States: Identifying Opportunities for Increased Utilization
1Saint Louis University, St. Louis, MO, 2U Iowa, Iowa City, IA, 3U Pittsburgh, Pittsburgh, PA, 4U Penn, Philadelphia, PA, 5UAB, Birmingham, AL, 6Yale, New Haven, CT, 7UNOS, Richmond, VA
Meeting: 2022 American Transplant Congress
Abstract number: 135
Keywords: African-American, Liver transplantation, Living donor, Multivariate analysis
Topic: Clinical Science » Liver » 58 - Liver: Living Donor Liver Transplant and Partial Grafts
Session Information
Session Name: Surgery innovative Techniques Including Living Donor
Session Type: Rapid Fire Oral Abstract
Date: Sunday, June 5, 2022
Session Time: 5:30pm-7:00pm
 Presentation Time: 6:10pm-6:20pm
Presentation Time: 6:10pm-6:20pm
Location: Hynes Room 313
*Purpose: To assess barriers to living donor liver transplant (LDLT) access in light of convincing evidence of survival benefits for patients with end-stage liver disease.
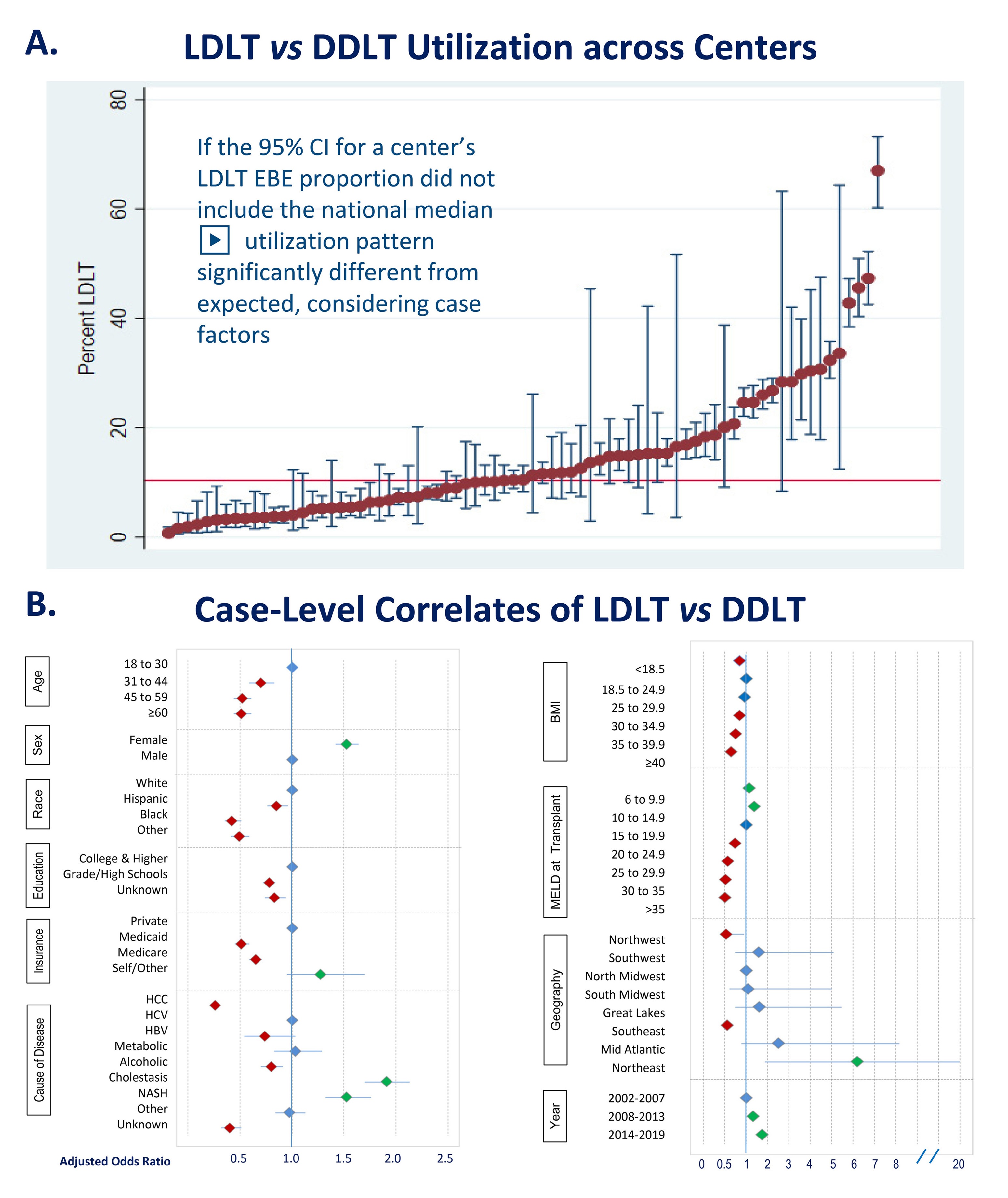
*Methods: We examined SRTR data to assess characteristics associated with receipt of an LDLT compared with a deceased donor liver transplant (DDLT) among US transplant centers that performed at least one LDLT in 2012-2019. Hierarchal regression modeling was used to quantify the impact of patient factors, center, geography, and temporal trends on the adjusted odds ratio (aOR) of undergoing LDLT (vs DDLT), at centers with established clinical experience.
*Results: Among 73,681 liver transplant recipients, only 12% received LDLT at the average center, although LDLT proportions varied from 1% to 20% across centers (Fig A).
After adjustment for center and patient factors, the likelihood of receiving an LDLT rose 73% in recent years (aOR, 1.73 for 2014-19 vs 2002-07). After accounting for center-level differences, patient characteristics dramatically affected access to LDLT. Older adults (vs. those aged 18 to 30), men (versus women), and racial/ethnic minorities (vs. White patients) were markedly less likely to undergo LDLT. (Fig B). When compared with transplant for hepatitis C, LDLT was less common in patients with hepatocellular carcinoma and alcoholic cirrhosis but more frequent in those with NASH. As expected, LDLT use was lower in patients outside of normal BMI limits. LDLT use was also higher with model for end-stage liver disease (MELD) less than 15 and declined with MELD 20 or higher. Socioeconomic status dramatically affected access to LDLT, with decreased use for patients with public insurance (vs. private) and lower educational achievement (vs. college or higher). Finally, the risk-adjusted LDLT proportion was lower in the Northwest and Southeast United States and higher in the Northeast (vs. Midwest).
*Conclusions: Despite established benefits and growing utilization, access to LDLT for patients with comparable illness severity is not equitable, as older patients and those with lower social determinants of health (educational achievement and public insurance) are less likely to receive LDLT. Further work is needed to assess the impact of donor availability and center practice on LDLT access and ensure its availability for all patients with clinically appropriate indications.
To cite this abstract in AMA style:
Lentine K, Axelrod D, Schnitzler M, Li R, Dew M, Bitterman T, Olthoff K, Locke J, Emre S, Hunt H, Tanaka T, Liapakis A. Variation in Adult Living Donor Liver Transplantation in the United States: Identifying Opportunities for Increased Utilization [abstract]. Am J Transplant. 2022; 22 (suppl 3). https://atcmeetingabstracts.com/abstract/variation-in-adult-living-donor-liver-transplantation-in-the-united-states-identifying-opportunities-for-increased-utilization/. Accessed February 21, 2026.« Back to 2022 American Transplant Congress