Utilization of Living Donor Liver Transplant for Patients Who Travel for Transplant in the United States
University of California, San Francisco, San Francisco, CA
Meeting: 2021 American Transplant Congress
Abstract number: 715
Keywords: Allocation, Ethics, Liver, Living donor
Topic: Clinical Science » Ethics » Non-Organ Specific: Economics & Ethics
Session Information
Session Name: Non-Organ Specific: Economics & Ethics
Session Type: Poster Abstract
Session Date & Time: None. Available on demand.
Location: Virtual
*Purpose: We have previously shown that United States (US) liver transplant (LT) candidates listed at a single center (SL) are disadvantaged compared with patients who travel for transplant—SL wait longer and have poorer post-transplant outcomes. SL compete for LT with multiply listed (ML) who are US citizens listed at more than one center, non-citizen, non-residents (NCNR) who travel to the US temporarily, and non-citizen, residents (NC-R) who travel to and reside in the US. This study aimed to examine living donor liver transplant (LDLT) recipients only in order to determine the impact of traveler status on outcomes in this subset of LT recipients.
*Methods: UNOS LT recipients from January 1, 2003-June 10, 2019 were reviewed, excluding re-transplant, pediatric, and multiple organ recipients. SL patients had one listing. ML patients had overlapping listing dates prior to transplant. NCNR and NC-R patients were defined by citizenship. Demographics were compared using descriptive statistics. Graft and patient survival were evaluated using the Kaplan Meier method and Cox PH.
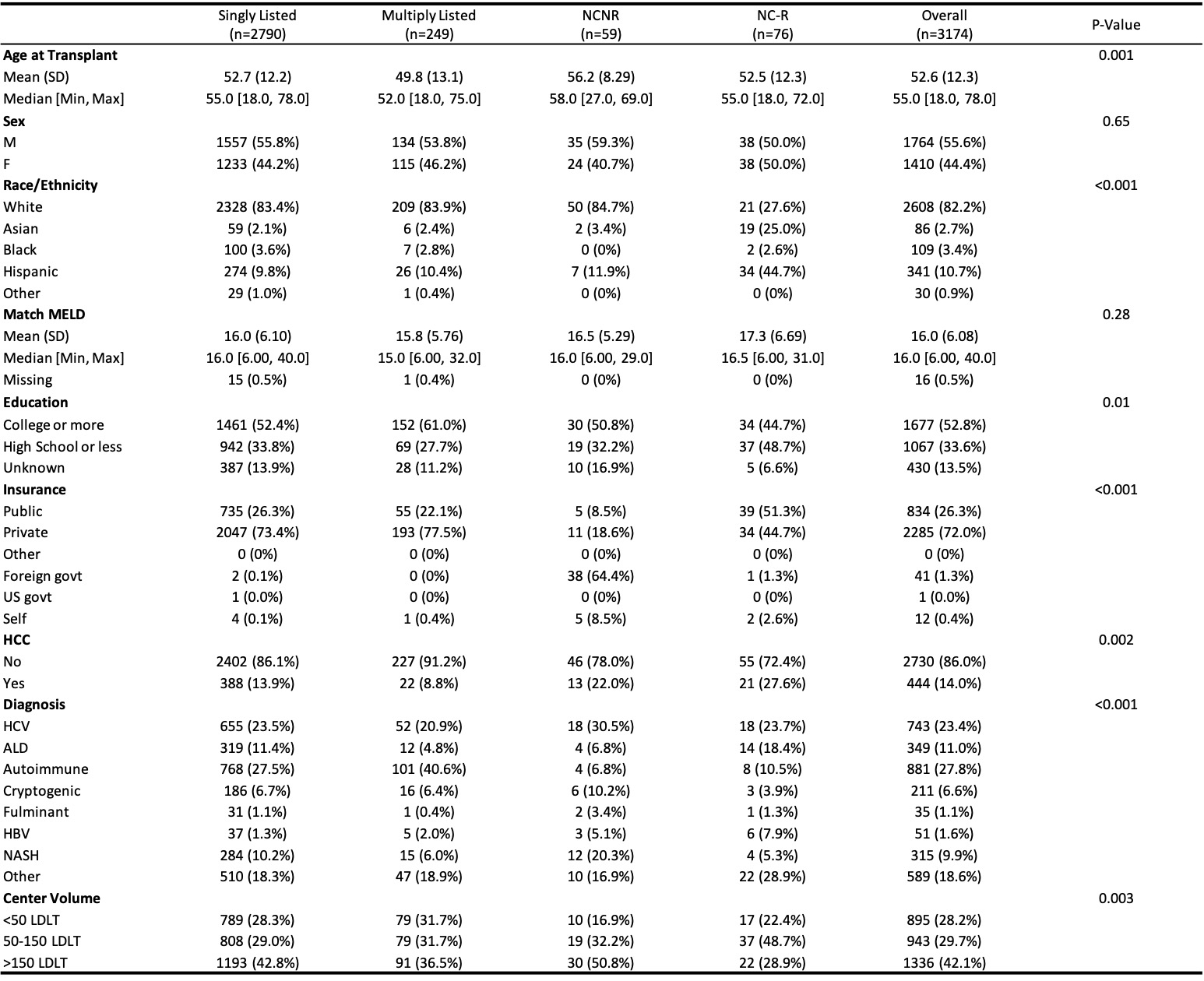
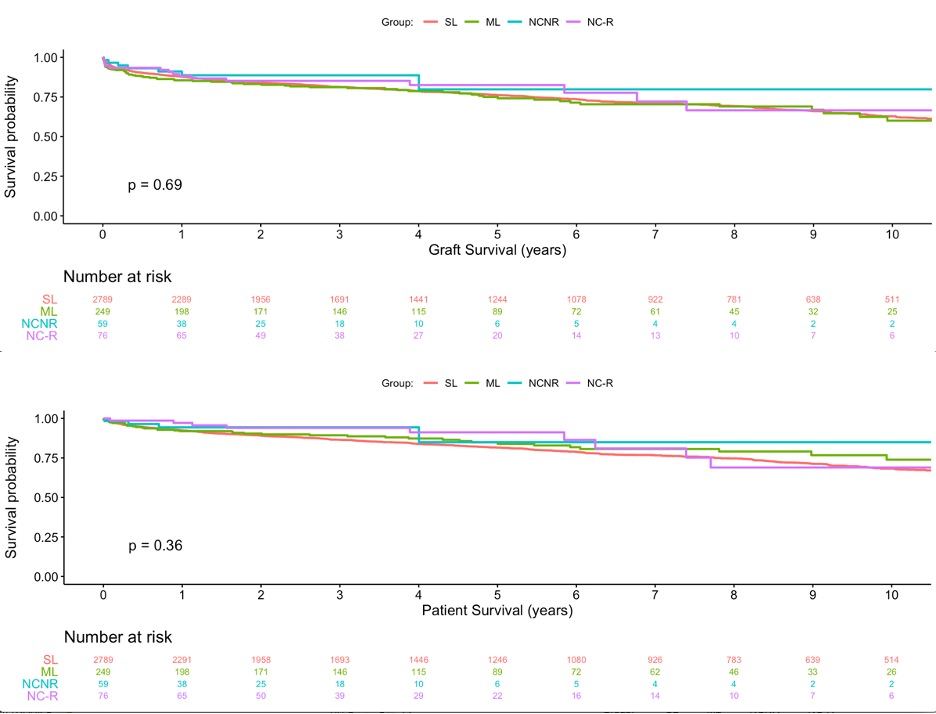
*Results: 75, 955 LT were performed during the study period, of which 3174 (4.1%) were LDLT. LDLT utilization in the four groups was significantly different (4.1% SL, 5.6% ML, 8.3% NCNR, 3.2% NC-R, p<0.001). There were significant demographic differences across the four groups in all variables except sex and match MELD (Figure 1). There was no significant difference in graft or patient survival when stratified by travel group (Figure 2). In a multivariable Cox model examining patient survival, only increasing age (HR 1.02, p-value<0.001) and presence of HCC (HR 1.59, p-value <0.001) were associated with increased risk of death after transplant.
*Conclusions: LDLT is most frequently utilized in NCNR and ML. Our findings suggest that LDLT may serve a dual purpose: 1) enabling LT in patients who travel for transplant while supporting self sufficiency by leaving the deceased donor pool intact, 2) equalizing post-transplant outcomes among all groups. These results highlight a need to identify barriers to LDLT among SL, and remind us that live donor protection and safety remains of paramount importance as we advocate for expanded use of LDLT.
To cite this abstract in AMA style:
Braun HJ, Amara D, Shui AM, Stock P, Hirose R, Delmonico F, Ascher NL. Utilization of Living Donor Liver Transplant for Patients Who Travel for Transplant in the United States [abstract]. Am J Transplant. 2021; 21 (suppl 3). https://atcmeetingabstracts.com/abstract/utilization-of-living-donor-liver-transplant-for-patients-who-travel-for-transplant-in-the-united-states/. Accessed March 1, 2026.« Back to 2021 American Transplant Congress