Utilization of HCV-Positive Donors' Kidneys: Potential Benefits in the Era of Direct Acting Antiviral (DAA) Therapy.
1Massachusetts General Hospital, Boston, MA
2Massachusetts General Hospital, Boston, MA
3Brigham and Women's Hospital, Boston, MA.
Meeting: 2016 American Transplant Congress
Abstract number: 75
Keywords: Cadaveric organs, Donation, Hepatitis C, Kidney transplantation
Session Information
Session Name: Concurrent Session: SOT: HIV, HBV, & HCV
Session Type: Concurrent Session
Date: Sunday, June 12, 2016
Session Time: 2:30pm-4:00pm
 Presentation Time: 3:42pm-3:54pm
Presentation Time: 3:42pm-3:54pm
Location: Room 313
Organ shortage and expanding kidney waiting list fostered utilization of HCV positive donors' organs (HCVD+). HCVD+ kidneys have slightly worse long term outcomes compared with HCV- kidneys, but better outcomes compared to remaining on the waiting list. Using HCVD+ for HCV+ patients may shorten waiting times decreasing its mortality. Limited early data of novel HCV DAA therapy in this population is promising, and may improve HCVD+ outcome.
To evaluate HCVD+ kidney utilization and post-transplant HCV therapy, we retrospectively reviewed charts of kidney transplant recipients between 1/1/2010 and 8/31/2015 at our institution.
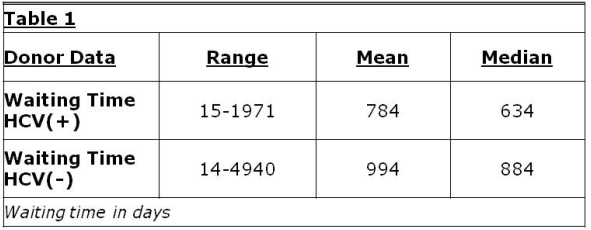
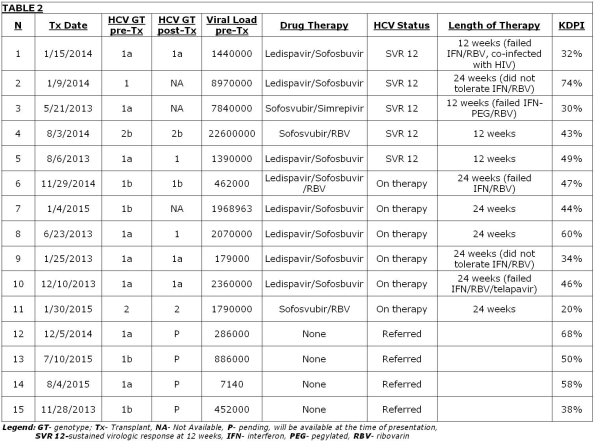
Multi-organ and living donor transplants were excluded. Of the remaining 305 deceased donor transplants, only 15 (5%) were from HCVD+. HCVD+ kidney recipients' had shorter waiting time and mean KDPI of 46% (Table1 and 2).
All of the HCVD+ kidney recipients have functioning allografts. Neither HCV genotype switches, nor new infections were noted among recipients. Eleven (73%) had HCV treated post transplant with DAA. Five of those (46%) achieved sustained virological response. Six remain on therapy. Four have not initiated treatment (Table2).
HCVD+ kidneys underutilization remains challenging at our institution and nationwide despite high quality of organs and documented good outcomes. According to Scientific Registry of Transplant Recipients, 2008-2012 data, 6.3% of deceased donor kidney recipients and 2.3% of deceased donors kidneys transplanted were HCV+, hence less than third of HCV+ recipients received HCVD+ kidneys.
With new highly effective DAA therapies, HCVD+ may represent a safe resource to expand the donor pool for HCV+ recipients.
CITATION INFORMATION: Amundsen B, Sise M, Lin M, Deirawan H, Heher E, Kimball B, Markmann J, Elias N. Utilization of HCV-Positive Donors' Kidneys: Potential Benefits in the Era of Direct Acting Antiviral (DAA) Therapy. Am J Transplant. 2016;16 (suppl 3).
To cite this abstract in AMA style:
Amundsen B, Sise M, Lin M, Deirawan H, Heher E, Kimball B, Markmann J, Elias N. Utilization of HCV-Positive Donors' Kidneys: Potential Benefits in the Era of Direct Acting Antiviral (DAA) Therapy. [abstract]. Am J Transplant. 2016; 16 (suppl 3). https://atcmeetingabstracts.com/abstract/utilization-of-hcv-positive-donors-kidneys-potential-benefits-in-the-era-of-direct-acting-antiviral-daa-therapy/. Accessed July 10, 2025.« Back to 2016 American Transplant Congress
