Utilization and Discard of HCV+ Donor Livers in the Advent of Direct-Acting Antiviral Therapy.
M. Bowring, L. Kucirka, A. Massie, X. Luo, M. Sulkowski, D. Segev, C. Durand.
JHU, Baltimore.
Meeting: 2016 American Transplant Congress
Abstract number: 262
Keywords: Donors, Hepatitis C, Liver, marginal
Session Information
Session Name: Concurrent Session: Viral Hepatitis
Session Type: Concurrent Session
Date: Monday, June 13, 2016
Session Time: 2:30pm-4:00pm
 Presentation Time: 2:30pm-2:42pm
Presentation Time: 2:30pm-2:42pm
Location: Ballroom A
While 45% of liver candidates are hepatitis C (HCV)-antibody positive (+) and might benefit from a HCV+ donor liver, only a small proportion receive one. The introduction of direct-acting antivirals (DAAs) in 2011 and interferon-free DAAs in 2013 dramatically improved outcomes for individuals with HCV. We explored changes in utilization and outcomes associated with HCV+ donor livers for HCV+ recipients.
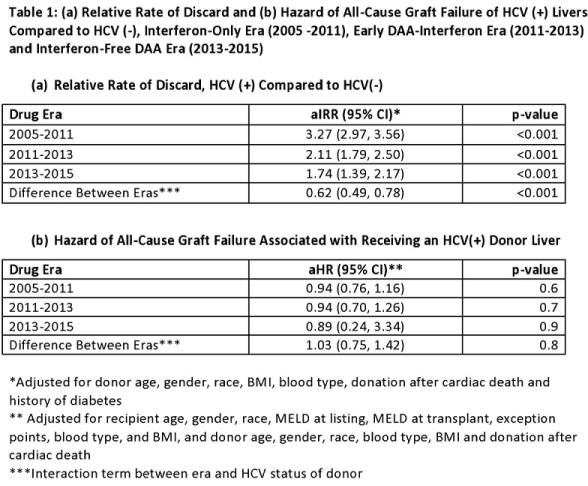
Methods: Using SRTR data 2005-2015, we studied 23,376 adult HCV+ recipients, using modified Poisson regression to estimate the relative rate (RR) of receiving a HCV+ liver, and Cox regression to estimate post-transplant survival associated with receiving a HCV+ donor liver, adjusting for recipient and donor characteristics.
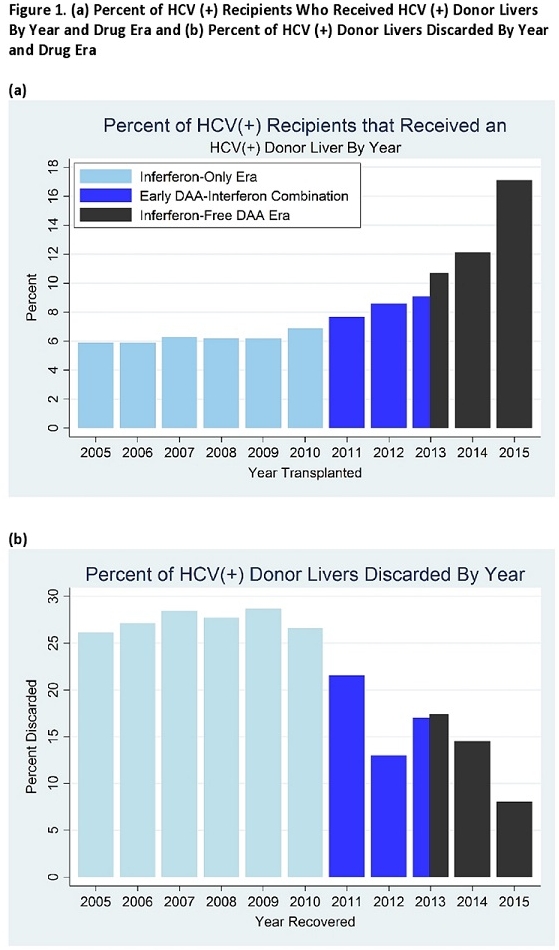
Results: The proportion of HCV+ recipients who received HCV+ livers increased from 6.9% in 2010 to 17.1% in 2015. HCV+ recipients were 29% more likely to receive a HCV+ liver after 2011 [aRR versus 2010: 1.141.291.46, p<0.001] and twice as likely to receive one after 2013 [aRR versus 2010: 1.792.042.23, p<0.001]. The discard rate of HCV+ livers declined from 26.6% in 2010 [aRR versus HCV- livers: 2.973.273.56,p<0.001] to 8.0% in 2015 [aRR versus HCV- livers: 1.391.742.17, p<0.001]. There was no difference in all-cause graft loss between HCV+ recipients of HCV+ and HCV- livers (aHR=0.93, p=0.4), and this did not change over time(p=0.8).
Conclusion: The utilization of HCV+ livers among HCV+ recipients has increased over time, particularly since the introduction of highly effective HCV therapies, yet post-transplant outcomes have not been negatively impacted. Despite this, HCV+ livers continue to be discarded at almost twice the rate of comparable HCV-negative livers. Increased utilization could expand the liver supply and improve outcomes for HCV+ transplant candidates.
CITATION INFORMATION: Bowring M, Kucirka L, Massie A, Luo X, Sulkowski M, Segev D, Durand C. Utilization and Discard of HCV+ Donor Livers in the Advent of Direct-Acting Antiviral Therapy. Am J Transplant. 2016;16 (suppl 3).
To cite this abstract in AMA style:
Bowring M, Kucirka L, Massie A, Luo X, Sulkowski M, Segev D, Durand C. Utilization and Discard of HCV+ Donor Livers in the Advent of Direct-Acting Antiviral Therapy. [abstract]. Am J Transplant. 2016; 16 (suppl 3). https://atcmeetingabstracts.com/abstract/utilization-and-discard-of-hcv-donor-livers-in-the-advent-of-direct-acting-antiviral-therapy/. Accessed February 26, 2026.« Back to 2016 American Transplant Congress
