Using Multidimensional Quality of Life Measurement to Better Understand the Benefit of Living Donor Kidney Transplant
Northwestern University, Chicago, IL
Meeting: 2019 American Transplant Congress
Abstract number: A169
Keywords: Quality of life
Session Information
Session Name: Poster Session A: Biomarkers, Immune Monitoring and Outcomes
Session Type: Poster Session
Date: Saturday, June 1, 2019
Session Time: 5:30pm-7:30pm
 Presentation Time: 5:30pm-7:30pm
Presentation Time: 5:30pm-7:30pm
Location: Hall C & D
*Purpose: Patient and graft survival after living donor kidney transplant (LDKT) are generally excellent, but there remains some variation in health-related quality of life (HRQOL) after LDKT. Additional information regarding changes in physical, mental/emotional, and social HRQOL from pre-to post-LDKT can help identify patient subgroups in need of attention.
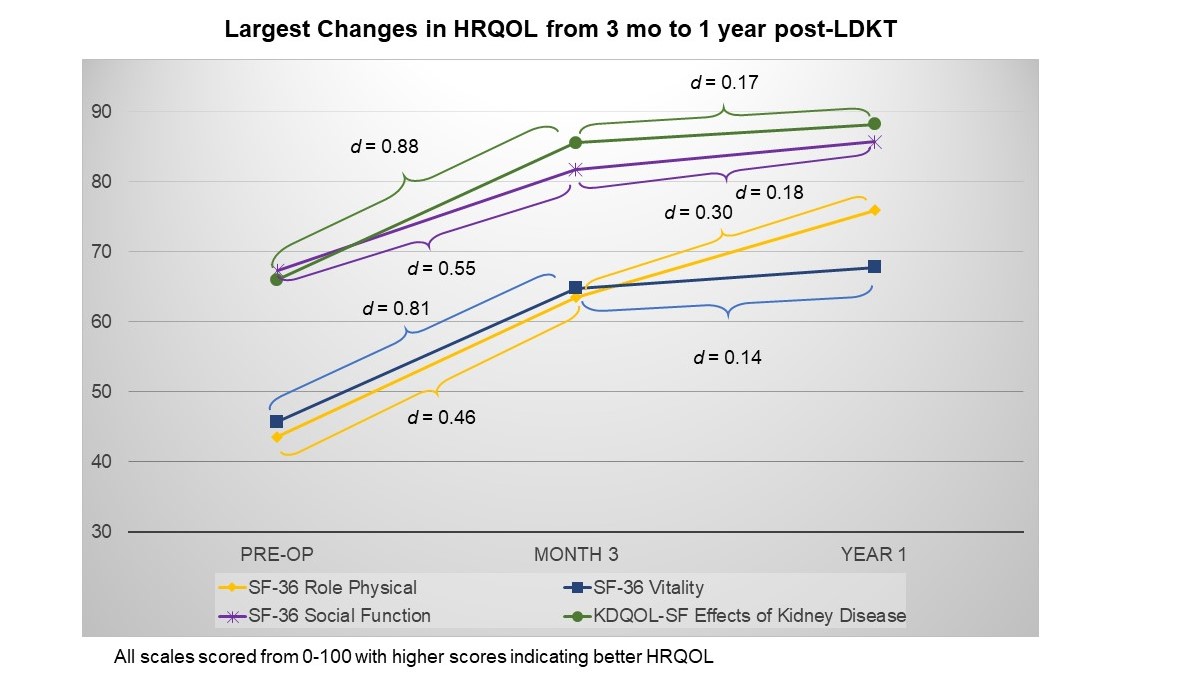
*Methods: For 477 patients transplanted between 11/2007 and 08/2016, we examined HRQOL before LDKT (pre-op), as well as 3 months and 1 year after LDKT. We used the SF-36 and the Kidney Disease Quality of Life – Short Form (KDQOL-SF) to examine changes in physical HRQOL (7 scales), mental/emotional HRQOL (4 scales), social HRQOL (4 scales), general health (1 scale), and kidney targeted HRQOL (3 scales). For each HRQOL scale, scores range between 0-100 and higher scores indicate better HRQOL. Using mixed effects models, we examined trajectories of each HRQOL domain. Standardized effect sizes (d) were calculated as the mean difference between time points divided by standard deviation of the change score. The following pre-specified cut-offs were used: 0.20 < d < 0.50 = small effect; 0.50 < d < 0.80 = medium effect; > 0.80 = large effect.
*Results: The largest effects were observed from pre-op to 3 mo post-LDKT and on the kidney-targeted HRQOL scales: KDQOL Effects of Kidney Disease (pre-op to 3 mo d=0.88, 3 mo to 1 yr d=0.17). (plot) In addition, the SF-36 Vitality scale increased at a large magnitude from pre-op to 3 mo (d=0.81). The SF-36 physical role limitations scale improved at a small but noteworthy magnitude from pre-op to 3 mo (d=0.46), as well as from 3 mo to 1 yr (d=0.30). Only one scale in the mental/emotional (SF-12 Mental Health Component Summary; pre-op to 3 mo d=0.53, 3 mo to 1 yr d=-0.05) and social HRQOL domains (SF-36 Social Function; pre-op to 3 mo d=0.55, 3 mo to 1 yr d=0.18) increased by a medium magnitude. In multivariable mixed effects models, lower creatinine, female gender, and non-white race were consistently associated with smaller increases in HRQOL across multiple scales.
*Conclusions: The largest gains in HRQOL were observed in the first 3 mo after LDKT, and are highest in patient-perceived impact of kidney disease. Clinical HRQOL surveillance may help target patients who appear to benefit less from LDKT for interventions.
To cite this abstract in AMA style:
Peipert J, Caicedo-Ramirez J, Ensor K, Friedewald J, Abecassis M, Cella D, Butt Z, Ladner D. Using Multidimensional Quality of Life Measurement to Better Understand the Benefit of Living Donor Kidney Transplant [abstract]. Am J Transplant. 2019; 19 (suppl 3). https://atcmeetingabstracts.com/abstract/using-multidimensional-quality-of-life-measurement-to-better-understand-the-benefit-of-living-donor-kidney-transplant/. Accessed February 15, 2026.« Back to 2019 American Transplant Congress