Use of Integrated National Registry and Pharmacy Claims Data to Identify Diabetes Mellitus After Live Pancreas Donation.
1Scientific Registry of Transplant Recipients, Minneapolis
2Univ Alberta, Alberta, Canada
3Dartmouth, Hanover
4Johns Hopkins, Baltimore
5Symphony Health, Pittsburgh
6Western Univ, London, Canada
7Washington Univ, St. Louis
8Saint Louis Univ, St. Louis.
Meeting: 2016 American Transplant Congress
Abstract number: A53
Keywords: Donation, Outcome, Pancreas, Post-operative complications
Session Information
Session Name: Poster Session A: Clinical Pancreas Transplantation and All Islet Cell Transplantation Topics
Session Type: Poster Session
Date: Saturday, June 11, 2016
Session Time: 5:30pm-7:30pm
 Presentation Time: 5:30pm-7:30pm
Presentation Time: 5:30pm-7:30pm
Location: Halls C&D
Living donor pancreas transplant is a potential treatment for diabetic patients with end-organ complications. Early post-donation surgical risks of living pancreas donation have been reported, but long-term outcomes are unknown. Increased risk of post-donation diabetes mellitus (PDDM) from pancreas insufficiency is a possible complication.
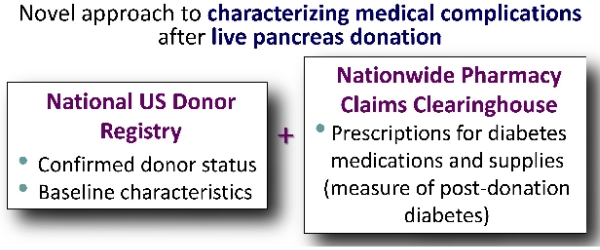
We integrated national Scientific Registry of Transplant Recipients data with records from a nationwide pharmacy claims warehouse to examine prescriptions for diabetic medications or supplies as a measure of PDDM.
Among 72 living pancreas donors registered in the US from 1988 to 2008, 45 were identified in the linked pharmacy database. Of these, 27% (12/45) filled prescriptions for diabetes treatments after donation. Among those with evidence of PDDM, the first pharmacy claim for a diabetes treatment occurred at an average of 14.3 yrs post-donation (average age at treatment, 51.9 yrs). There were no significant associations of PDDM with sex, race, ethnicity, blood type, or donor-recipient relationship, although power was limited by the sample size. Comparing living pancreas donors who developed PDDM and those did not, we did not find significant differences in age at donation (37.7 vs. 39.5 years, p=0.61) or era effects (yr of donation: 1996 vs. 1997, p=0.54).
Living pancreas donors develop PDDM at rates exceeding the general US population, among whom diabetes prevalence at age 45-64 yrs is 12.2%. The increased incidence of diabetes in pancreas donors compared with non-donors screened for baseline good health is likely to be higher. Integration of national registry and pharmacy data is a novel strategy for assessing otherwise unmeasured health outcomes among small groups in transplantation.
CITATION INFORMATION: Lentine K, Lam N, Randall H, Axelrod D, Segev D, Hess G, Garg A, Brennan D, Kasiske B, Schnitzler M. Use of Integrated National Registry and Pharmacy Claims Data to Identify Diabetes Mellitus After Live Pancreas Donation. Am J Transplant. 2016;16 (suppl 3).
To cite this abstract in AMA style:
Lentine K, Lam N, Randall H, Axelrod D, Segev D, Hess G, Garg A, Brennan D, Kasiske B, Schnitzler M. Use of Integrated National Registry and Pharmacy Claims Data to Identify Diabetes Mellitus After Live Pancreas Donation. [abstract]. Am J Transplant. 2016; 16 (suppl 3). https://atcmeetingabstracts.com/abstract/use-of-integrated-national-registry-and-pharmacy-claims-data-to-identify-diabetes-mellitus-after-live-pancreas-donation/. Accessed February 24, 2026.« Back to 2016 American Transplant Congress
