Unplanned Pregnancies after Liver Transplant Are Associated with Adverse Pregnancy Outcomes
1Medicine, University of California San Francisco, San Francisco, PA, 2Gift of Life Institute, Transplant Pregnancy Registry International, Philadelphia, PA, 3Medicine, University of Virginia Health System, Charlottesville, VA, 4Medicine, Lewis Katz Temple University School of Medicine, Philadelphia, PA, 5Surgery, Lehigh Valley Health Network, Allentown, PA
Meeting: 2019 American Transplant Congress
Abstract number: B315
Keywords: High-risk, Liver transplantation, Pregnancy, Quality of life
Session Information
Session Name: Poster Session B: Liver Retransplantation and Other Complications
Session Type: Poster Session
Date: Sunday, June 2, 2019
Session Time: 6:00pm-7:00pm
 Presentation Time: 6:00pm-7:00pm
Presentation Time: 6:00pm-7:00pm
Location: Hall C & D
*Purpose: The purpose of this study is to analyze planned vs. unplanned pregnancies in female liver transplant recipients. Background: Over 30% of female transplant patients are reproductive aged and fertility is rapidly restored following liver transplant. Pregnancy post-transplant is considered higher risk, therefore careful pre-conception management is advised. However, data on prevalence of unplanned pregnancies are lacking, including their potential association with adverse maternal and fetal outcomes.
*Methods: Data were collected by the Transplant Pregnancy Registry International (TPR), a voluntary pregnancy registry using questionnaires, telephone interviews, and medical records review. Maternal, fetal, and transplant outcomes were compared between women who self-reported planned versus unplanned pregnancies.
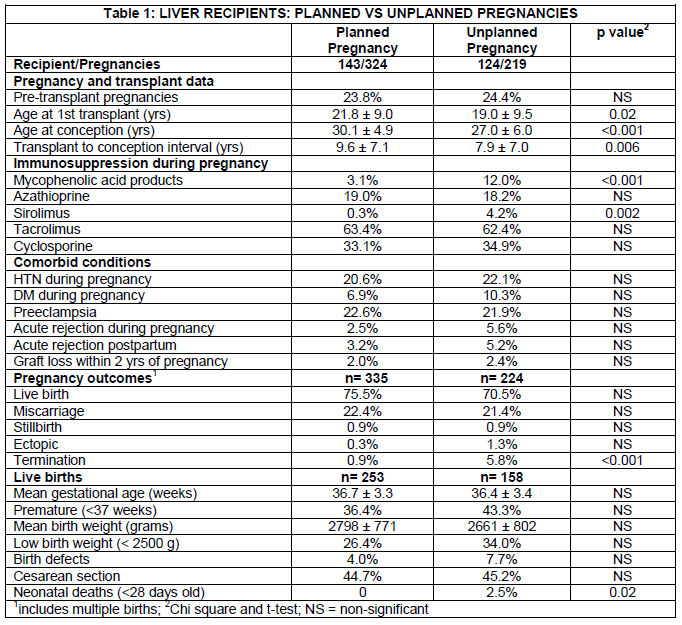
*Results: Data from 543 pregnancies were analyzed with conception dates from Nov 1985-May 2018, of which 40% were unplanned. The median age at both transplant and conception was younger for unplanned pregnancies, and these women had a shorter transplant to conception interval (Table).
In unplanned pregnancies the fetus was more likely to be exposed to MPA agents (12.0 vs 3.1%, p<0.001). Although no significant differences were noted for maternal outcomes, diabetes (10.0 vs 7%) and acute rejection (5.6 vs 2.5%) were numerically more common in the unplanned group. Pregnancy termination (5.8 vs 0.6%) and neonatal deaths (2.5 vs 0%) were significantly more common with unplanned pregnancy. Although not statistically significant, there were higher rates of infants born with birth defects (7.7 vs 4.0%), prematurity (43.3 vs 36.4%), and/or low birth weight (34.0 vs 26.4%).
*Conclusions: In this large pregnancy cohort of liver transplant recipients we identified a high prevalence of unplanned pregnancy at ~40%. Unplanned pregnancies were more common in younger women and associated with pregnancy termination as well as neonatal death. Exposure to the teratogenic MPA agents was also higher in unplanned pregnancies. Improvement in contraception and pre-conception counseling are imperative for reducing the high number of unplanned pregnancies in liver transplant recipients, and to improving their overall reproductive care.
To cite this abstract in AMA style:
Sarkar M, Coscia LA, Kliniewski D, Rao S, Constantinescu S, Moritz MJ. Unplanned Pregnancies after Liver Transplant Are Associated with Adverse Pregnancy Outcomes [abstract]. Am J Transplant. 2019; 19 (suppl 3). https://atcmeetingabstracts.com/abstract/unplanned-pregnancies-after-liver-transplant-are-associated-with-adverse-pregnancy-outcomes/. Accessed February 26, 2026.« Back to 2019 American Transplant Congress