Tracheostomy Following Liver Transplantation
Surgery, University of Illinois at Chicago, Chicago, IL
Meeting: 2019 American Transplant Congress
Abstract number: C362
Keywords: Liver transplantation, Resource utilization, Surgical complications, Trachea
Session Information
Session Name: Poster Session C: Surgical Issues: All Organs
Session Type: Poster Session
Date: Monday, June 3, 2019
Session Time: 6:00pm-7:00pm
 Presentation Time: 6:00pm-7:00pm
Presentation Time: 6:00pm-7:00pm
Location: Hall C & D
*Purpose: With the current demand for liver transplantation, sicker patients are frequently transplanted. These patient are at a higher risk of significant morbidity following surgery, including respiratory failure. This study evaluated the phenotype that characterizes liver transplant candidates that may benefit from early tracheostomy.
*Methods: A single center retrospective review of all liver transplant candidates. Patients who eventually required tracheostomies were identified and compared to their counterparts. Ventilatory parameters and patient characteristics were compared.
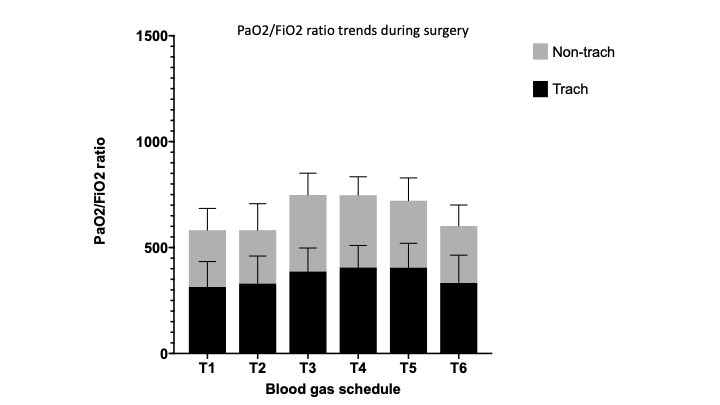
*Results: Of the 130 liver transplants performed between January 2012 and December 2017, 11 patients required tracheostomy. Although the patients in the tracheostomized population (TP) did not have significantly worse preoperative functional status (< 4 metabolic equivalents; 64% vs 42%, p=0.21), patients who required tracheostomies did have a greater native MELD score (37 vs 30, p<0.05), at the time of transplantation. When comparing intra-operative characteristics, patient who eventually succumbed to respiratory failure had decreased PaO2/FiO2 ratios at the start of surgery and remained significantly lower for the duration of surgery compared to the non-tracheostomy group (p <0.05). TP patients required more net fluid resuscitation intra-operatively (7.3 vs 5.0 liters, p<0.05), increased length of time to attempted extubation (3.5 vs 1 day, p<0.05), longer mechanical ventilation days (15 vs 1 day, p<0.05), increased length of stay (37 vs 9 days, p<0.05) and higher 1-year mortality (36% vs 8%, p<0.05).
*Conclusions: After reviewing the pre-operative and intra-operative data, patients with a high MELD score (>30), net post-operative fluid balance > 5L, and PaO2/FiO2 ratio ≤ 300 who fail to wean off mechanical ventilation after 72 hours may benefit from tracheostomy during the post-operative period.
To cite this abstract in AMA style:
Almario J, Okoye O, Spaggiari M, Jacob K, Cocco PDi, Benedetti E, Tzvetanov I. Tracheostomy Following Liver Transplantation [abstract]. Am J Transplant. 2019; 19 (suppl 3). https://atcmeetingabstracts.com/abstract/tracheostomy-following-liver-transplantation/. Accessed March 12, 2026.« Back to 2019 American Transplant Congress