Tracheostomy After Liver Transplantation: Utility and Impact
Liver and Pancreas Transplant Center, UCLA, Los Angeles, CA
Meeting: 2022 American Transplant Congress
Abstract number: 522
Keywords: Liver transplantation, Post-operative complications, Risk factors, Trachea
Topic: Clinical Science » Liver » 51 - Liver: Retransplantation and Other Complications
Session Information
Session Name: Retransplantation and Other Complications
Session Type: Rapid Fire Oral Abstract
Date: Tuesday, June 7, 2022
Session Time: 5:30pm-7:00pm
 Presentation Time: 6:20pm-6:30pm
Presentation Time: 6:20pm-6:30pm
Location: Hynes Room 313
*Purpose: High acuity Liver transplant (LT) patients have an increased risk of postoperative respiratory failure requiring tracheostomy (TS). The use of TS in ventilator-dependent patients after LT remains variable with limited data in this patient population. The aim of this study is to evaluate clinical predictors for post-LT TS requirement, and investigate outcome predictors in patients with TS after LT.
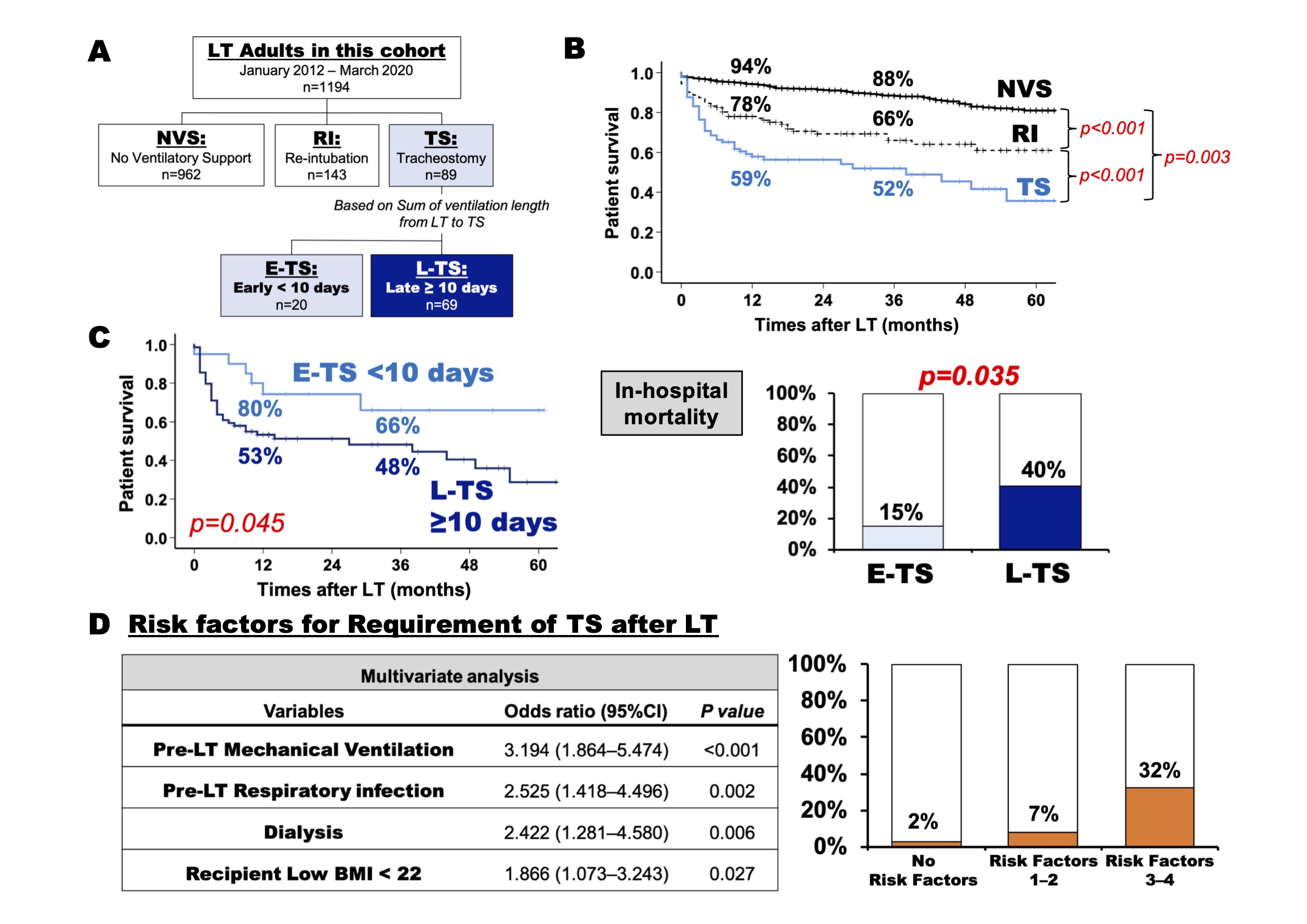
*Methods: Adult LT recipients at our institution between January 2012 and March 2020 were retrospectively reviewed. Patients who had TS preoperatively were excluded. Post LT patients were divided into three groups, those requiring no ventilatory support (NVT) post LT, those needing re-intubation (RI) alone, and patients requiring TS. Patients with TS were sub-divided into early [E-TS] and late [L-TS] groups based on sum of ventilation length in days from LT to TS (Fig A). Survival and multivariate analysis were performed to identify risk factors for TS requirement after LT.
*Results: Of 1194 patients analyzed (Medain MELD 34), 89 patients (7%) (Median MELD 39) required post-LT TS for prolonged respiratory failure. Patients with TS had the lowest post-LT patient survival rate compared with NVS and RI patients (1- and 3-year survival: 59%, 52% in TS, 94%, 88% in NVS, 78%, 66% in RI; Fig. B). Analysis of the sum of ventilation duration from LT to TS (Median 15 days [10-20]), identified 10 days as the cut-off point impacting survival outcome between E-TS (<10 days) and L-TS (≥10 days). E-TS was associated with better survival compared to L-TS (1- and 3-year survival: 80%, 66% vs. 53%, 48%, p=0.04; Fig. C). E-TS had significantly lower in-hospital mortality compared to L-TS (15 vs. 40%, p=0.03). Multivariate analysis identified pre-LT mechanical ventilation (p<0.001), respiratory infection (p=0.002), dialysis (p=0.006), and recipient low BMI (≤22, p=0.02) as independent risk factors for post-LT TS. These risk factors were additive and significantly correlated with increased incidence of post-LT TS (p<0.001; Fig. D).
*Conclusions: This is the largest single center series to date examining impact of post-LT respiratory failure requiring TS on outcomes. E-TS had better patient survival outcome and lower in-hospital mortality than L-TS. Independent risk factors for post-LT TS requirement may serve to guide peri-operative management in high acuity LT recipients.
To cite this abstract in AMA style:
Noguchi D, Nguyen VM, Rosenthal CJ, Agopian VG, Farmer DG, Kaldas FM. Tracheostomy After Liver Transplantation: Utility and Impact [abstract]. Am J Transplant. 2022; 22 (suppl 3). https://atcmeetingabstracts.com/abstract/tracheostomy-after-liver-transplantation-utility-and-impact/. Accessed February 23, 2026.« Back to 2022 American Transplant Congress