The Ultimate Calculated Panel Reactive Antibody Value Predicts Mortality After Heart Transplantation.
1Cedars-Sinai Heart Institute, Los Angeles
2Mayo Clinic Arizona, Phoenix
Meeting: 2017 American Transplant Congress
Abstract number: 38
Keywords: Antibodies, Heart/lung transplantation, Waiting lists
Session Information
Session Name: Concurrent Session: Heart Waitlist and Allocation: Working to Get It Right
Session Type: Concurrent Session
Date: Sunday, April 30, 2017
Session Time: 2:30pm-4:00pm
 Presentation Time: 3:30pm-3:42pm
Presentation Time: 3:30pm-3:42pm
Location: E267
Background: Sensitized heart transplant (HT) candidates are known to be at higher risk for adverse events after transplantation, including a positive crossmatch, rejection, and death. These candidates are known to have prolonged time on the waiting list (WL), during which their listed unacceptable human leukocyte antigens (UA-HLA) and thus their calculated panel reactive antibody value (CPRA) may change. We sought to determine the time point relative to HT that most strongly predicted post-HT mortality.
Methods: A dataset of patients listed for HT with UA-HLA between years (yrs) 1997-2016 were obtained from UNOS. Yrs that contained ≥1% of WL additions with UA-HLA as well as at least 1-yr follow-up were selected for further analysis (2006–2014). A CPRA calculator was developed using R (R Foundation for Statistical Computing, Vienna, Austria). CPRA was calculated for each candidate at each WL modification with UA-HLA. CPRA could not be calculated for 6 candidates. The initial, ultimate, minimum, mean, maximum, and union (i.e. all UA-HLA during listing) CPRA values were calculated. Cox proportional hazards analysis was performed using these metrics as potential predictors and 1-yr post-HT survival as the response variable.
Results:We identified 4,610 candidates with UA-HLA. Of these, 2,519(55%) underwent HT. The median number of WL modifications with UA-HLA was 7 (IQR 4 – 13). The CPRA increased during listing (from initial to ultimate CPRA) in 428(17%), decreased in 410(16%) and didn't change in 1,675(67%) candidates. After HT, 258(11%) recipients died within the first yr. The ultimate CPRA was a statistically significant predictor of survival at 1-yr post-HT, with a hazard ratio of 1.05 per 10% increase in CPRA (p=0.03), whereas the initial, minimum, mean, maximum, and total CPRA did not predict survival.
Conclusion: The ultimate CPRA, that is the CPRA measured immediately prior to HT, was the only CPRA variable that predicted mortality at 1-yr post-HT. These results suggest that periodic monitoring and updating of UA-HLA is necessary to accurately predict post-HT outcomes.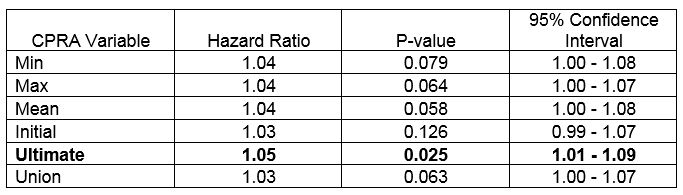
CITATION INFORMATION: Kransdorf E, Kittleson M, Patel J, Pando M, Czer L, Kobashigawa J. The Ultimate Calculated Panel Reactive Antibody Value Predicts Mortality After Heart Transplantation. Am J Transplant. 2017;17 (suppl 3).
To cite this abstract in AMA style:
Kransdorf E, Kittleson M, Patel J, Pando M, Czer L, Kobashigawa J. The Ultimate Calculated Panel Reactive Antibody Value Predicts Mortality After Heart Transplantation. [abstract]. Am J Transplant. 2017; 17 (suppl 3). https://atcmeetingabstracts.com/abstract/the-ultimate-calculated-panel-reactive-antibody-value-predicts-mortality-after-heart-transplantation/. Accessed March 3, 2026.« Back to 2017 American Transplant Congress
