The Relative Association of Clinical Variables and Histologic Lesions with Molecular Rejection in Kidney Transplant Biopsies
1University of Alberta, Edmonton, AB, Canada, 2Alberta Transplant Applied Genomics Centre, Edmonton, AB, Canada, 3INTERCOMEX, Edmonton, AB, Canada
Meeting: 2022 American Transplant Congress
Abstract number: 215
Keywords: Biopsy, Kidney transplantation, Rejection
Topic: Clinical Science » Kidney » 34 - Kidney: Acute Cellular Rejection
Session Information
Session Name: Kidney: Acute Cellular Rejection
Session Type: Rapid Fire Oral Abstract
Date: Monday, June 6, 2022
Session Time: 3:30pm-5:00pm
 Presentation Time: 4:50pm-5:00pm
Presentation Time: 4:50pm-5:00pm
Location: Hynes Ballroom A
*Purpose: Availability of molecular assessment (MMDx) independent of conventional variables (time, clinical, histologic, and HLA antibody) presents an opportunity to re-assess the relative strength of the association of each conventional variable with molecular rejection in multivariable models.
*Methods: Logistic regression selected the best histologic/clinical variables for diagnosing automatically assigned molecular archetype definitions of ABMR, TCMR, and any rejection in 1679 indication biopsies from the INTERCOMEX study. Input variables included standard histology lesions, DSA, PRA, C4d, and time of biopsy post-transplant (TxBx). TxBx was modelled as non-linear, using restricted cubic splines. Variable selection used backward elimination.
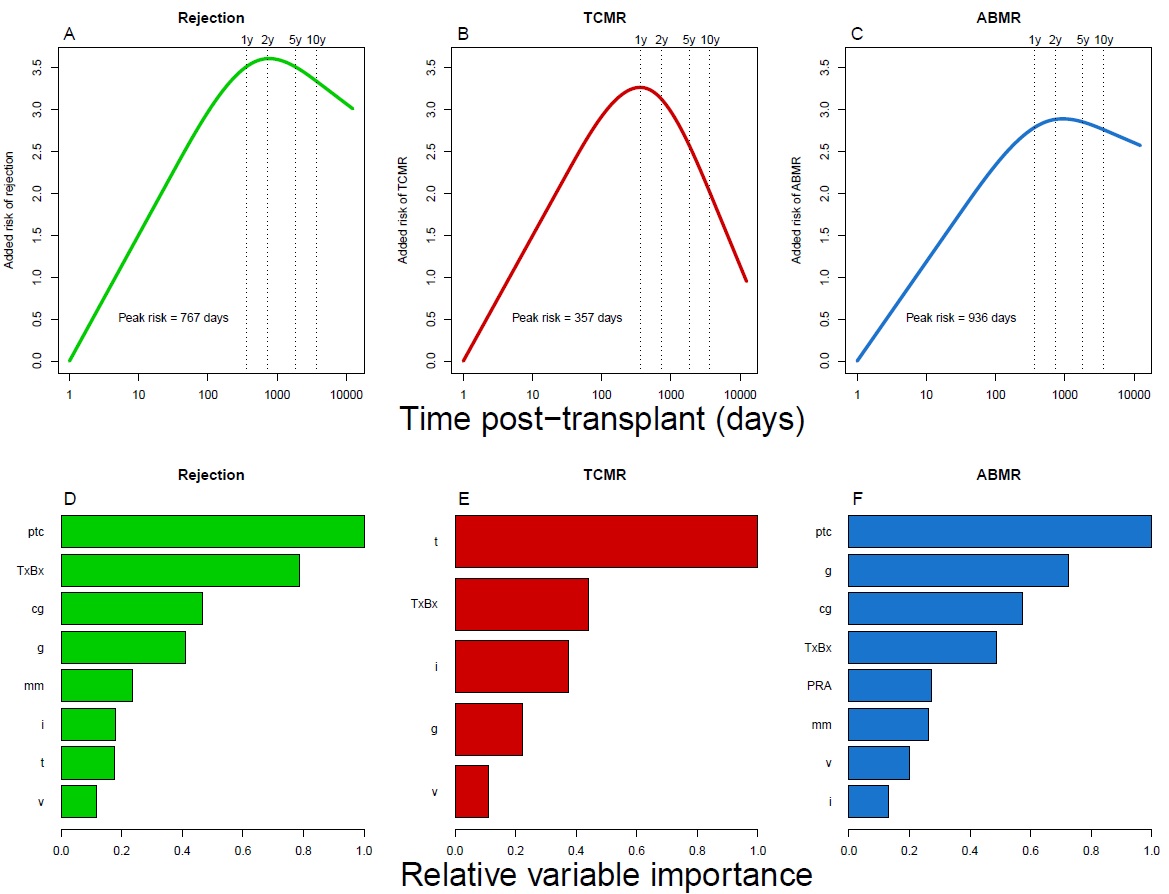
*Results: TxBx was a significant predictor of rejection. Time-associated risk of any rejection peaked at 767 days (Figure 1A). TCMR risk peaked at 316 days (Figure 1B), then sharply declined; ABMR peaked later 936 days (Figure 1 C) and was sustained. The models showed the relative strength of the association between histologic lesions and molecular diagnoses. In predicting any rejection (and thus no rejection) ptc and time were most important. HLA antibody status and v-lesions were relatively unimportant (Figure 1D) In predicting molecular TCMR, the importance of conventional variables was t-lesions > TxBx > i-lesions (Figure 1E). Increased g-lesion scores reduced the probability of TCMR. In predicting ABMR, the relative importance of conventional variables was ptc> g>cg>TxBx (Figure 1F). PRA status was important but DSA status and C4d were not (probably reflecting DSA-negative ABMR).
*Conclusions: Time post-transplant alone has value in predicting the findings in indication biopsies. The models confirm the dominant importance of t-lesions and TxBx in TCMR and of ptc, g, and cg, plus TxBx and PRA (not DSA or C4d) in ABMR. V-lesions are of relatively little importance.
To cite this abstract in AMA style:
Sikosana ML, Reeve J, Halloran PF, Investigators INTERCOMEX. The Relative Association of Clinical Variables and Histologic Lesions with Molecular Rejection in Kidney Transplant Biopsies [abstract]. Am J Transplant. 2022; 22 (suppl 3). https://atcmeetingabstracts.com/abstract/the-relative-association-of-clinical-variables-and-histologic-lesions-with-molecular-rejection-in-kidney-transplant-biopsies/. Accessed February 28, 2026.« Back to 2022 American Transplant Congress