The Relationship Between Frailty and Performance Status in Patients with Cirrhosis Awaiting Liver Transplantation
1Department of Medicine, UCSF, San Francisco, CA, 2Division of Gastroenterology and Hepatology, Department of Medicine, UCSF, San Francisco, CA
Meeting: 2020 American Transplant Congress
Abstract number: B-168
Keywords: Liver cirrhosis, Liver transplantation, Mortality, Waiting lists
Session Information
Session Name: Poster Session B: Liver: Recipient Selection
Session Type: Poster Session
Date: Saturday, May 30, 2020
Session Time: 3:15pm-4:00pm
 Presentation Time: 3:30pm-4:00pm
Presentation Time: 3:30pm-4:00pm
Location: Virtual
*Purpose: Frailty—a multi-dimensional construct that encapsulates physical function, performance status, and nutritional status—has emerged as a critical determinant of mortality in patients with cirrhosis. Currently, the UNOS registry only includes the Karnofsky Performance Status (KPS) scale, which captures only one single component of frailty. We aimed to evaluate the relationship between frailty and KPS.
*Methods: We analyzed data from adults with cirrhosis listed for liver transplantation (LT) without hepatocellular carcinoma at a single center from 2/2014-6/2019 with outpatient assessments of frailty [using the Liver Frailty Index (LFI)] and performance status (using KPS) within 30 days of listing. “Frail” was defined using the previously established LFI cutoff of ≥4.5. Correlation between LFI and KPS was evaluated using Spearman’s correlation test. Uni- and sequential multivariable analyses assessed associations between LFI and KPS with waitlist mortality (= death/delisting for sickness) using competing risk models (with LT as the competing risk).
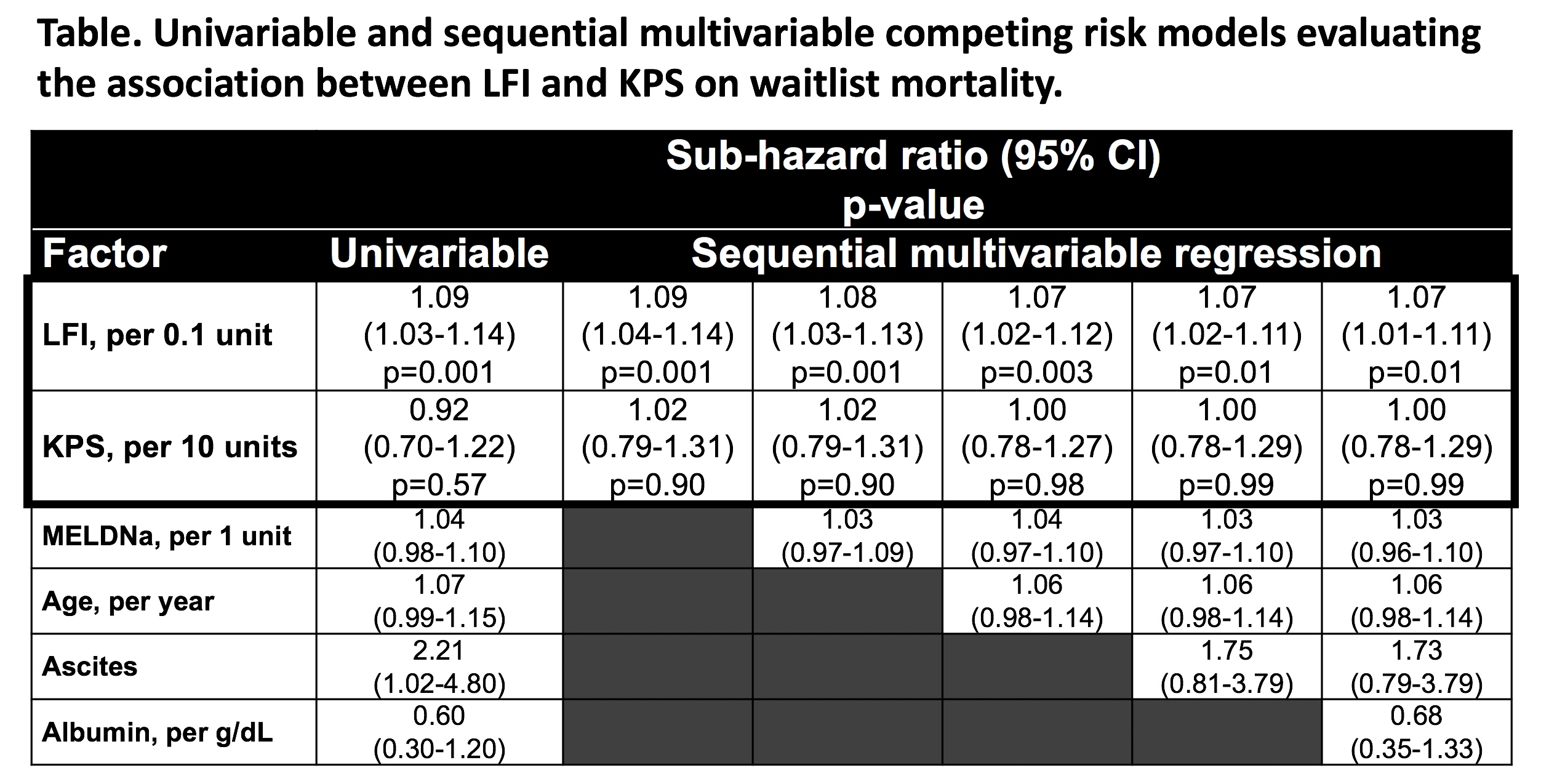
*Results: Included were 247 patients with cirrhosis: median MELDNa was 17. Median (IQR) LFI was 3.9 (3.4-4.5); median KPS was 80 (70-90). The correlation between LFI and KPS was -0.32 (p<0.001). Among 61 (25%) patients who were categorized as frail, median (IQR) KPS was 80 (60-90); 45% were modestly impaired (KPS 50-70) and 3% were severely impaired (KPS 10-40). At a median of 8 months follow-up, 25 (10%) patients died/were delisted. In univariable analysis, LFI (sHR 1.09, per 0.1 unit, 95% CI 1.03-1.14) was associated with waitlist mortality while KPS was not (sHR 0.92, per 10 units, 95% CI 0.70-1.22), which remained true in multivariable analysis (Table).
*Conclusions: Among patients with cirrhosis, there was only modest correlation between frailty and performance status. While frailty was predictive of waitlist mortality in our outpatient cohort of LT candidates with a median MELDNa of 17, KPS was not. Our data provide evidence that KPS does not fully capture “frailty” in outpatients with cirrhosis and suggest that frailty, as measured by the Liver Frailty Index, may be more appropriate to capture mortality risk than performance status alone and advocate for its incorporation into the UNOS registry.
To cite this abstract in AMA style:
Xu CQ, Yao F, Mohamad Y, Wong R, Kent D, Seetharaman S, Srisengfa Y, Lai JC. The Relationship Between Frailty and Performance Status in Patients with Cirrhosis Awaiting Liver Transplantation [abstract]. Am J Transplant. 2020; 20 (suppl 3). https://atcmeetingabstracts.com/abstract/the-relationship-between-frailty-and-performance-status-in-patients-with-cirrhosis-awaiting-liver-transplantation/. Accessed March 3, 2026.« Back to 2020 American Transplant Congress