The Oncological Influences of Pre- and Post-Transplant Sustained Viral Response in Liver Transplant for Hepatocellular Carcinoma
1Stanford University, Stanford, CA, 2Massachusetts General Hospital, Boston, MA, 3University of Rochester, Rochester, NY, 4Mount Sinai Medical Center, New York, NY, 5University of South Florida, Tampa, FL, 6Cleveland Clinic, Cleveland, OH
Meeting: 2022 American Transplant Congress
Abstract number: 1099
Keywords: Hepatitis C, Hepatocellular carcinoma, Liver transplantation
Topic: Clinical Science » Liver » 56 - Liver: Hepatocellular Carcinoma and Other Malignancies
Session Information
Session Name: Liver: Hepatocellular Carcinoma and Other Malignancies
Session Type: Poster Abstract
Date: Sunday, June 5, 2022
Session Time: 7:00pm-8:00pm
 Presentation Time: 7:00pm-8:00pm
Presentation Time: 7:00pm-8:00pm
Location: Hynes Halls C & D
*Purpose: Chronic hepatitis C infection (HCV) is one of the most common causes of hepatocellular carcinoma. After emerging direct-acting agents (DAA), the success rate of sustained viral response (SVR) is approximately 95%. Although, the eradication of HCV is a feasible option and survival benefit is obvious for liver transplant (LT) patients, the oncological benefit of SVR has not been fully elucidated to date. Especially, achieving SVR is beneficial to post-LT overall survival, which affects estimating the oncological influences of SVR in LT for HCC. This study aimed to investigate the influences of pre-and post-transplant SVR on tumor recurrence using a competing risk model.
*Methods: This was a multicenter study, which included 546 adult HCV patients with HCC who underwent LT between 2002-2020. The oncological benefits of achieving SVR were evaluated using the Fine and Gray competing risk model (event: recurrence, competing risk: non-cancer-related death). The oncological risk was defined as RETREAT score >3.
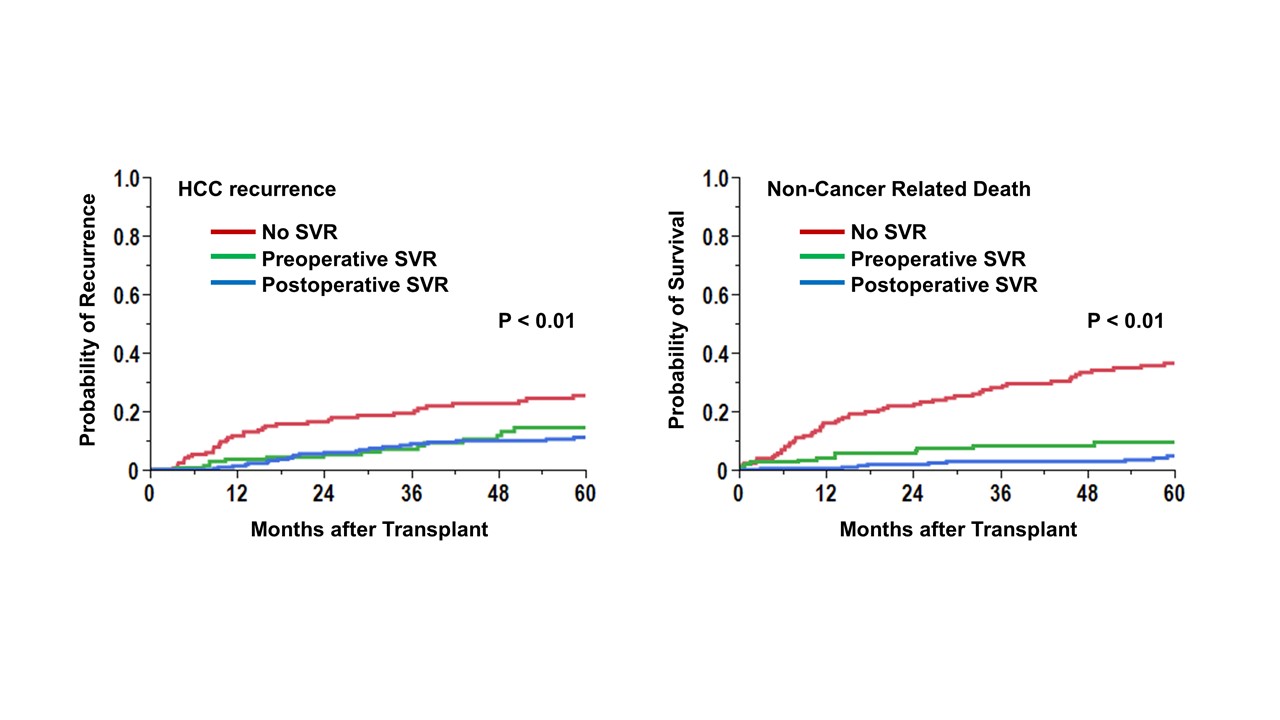
*Results: Of 546 HCV patients, 145 patients achieved SVR before transplant, and 228 patients achieved SVR after transplant. The cumulative incidence curves of recurrence and non-cancer-related death were shown (Figure). Achieving SVR reduced the risk of both HCC recurrence and non-cancer-related death compared to patients without SVR. The competing risk regression analyses showed achieving SVR reduced 24% (p=0.02) of recurrence risk and 38 % risk of non-cancer-related death. Of patients who achieved SVR, there was no significant difference according to the timing of achieving SVR (postoperative SVR; HR 0.67 (0.35-1.26), p=0.21). Interestingly, the HR of postoperative SVR was 0.50 (p=0.15) in low oncological risk patients and was 1.3 in the high oncological risk cohort (p=0.56).
*Conclusions: Achieving SVR reduces both cancer and non-cancer risk. The prognostic influence of SVR timing (pre-LT or post LT) is still controversial and possibly differ according to the oncological risk of recurrence.
To cite this abstract in AMA style:
Sasaki K, Kimura S, Tomiyama K, Bekki Y, Murray M, Huang P, Fruscione M, Moro A, Kwon C. The Oncological Influences of Pre- and Post-Transplant Sustained Viral Response in Liver Transplant for Hepatocellular Carcinoma [abstract]. Am J Transplant. 2022; 22 (suppl 3). https://atcmeetingabstracts.com/abstract/the-oncological-influences-of-pre-and-post-transplant-sustained-viral-response-in-liver-transplant-for-hepatocellular-carcinoma/. Accessed March 4, 2026.« Back to 2022 American Transplant Congress