The Impact of Insurance Status on Waiting List and Post-Lung Transplant Survival in Patients with Cystic Fibrosis.
1Cleveland Clinic, Cleveland, OH
2Scientific Reg of Transplant Recipients, Minneapolis, MN
Meeting: 2017 American Transplant Congress
Abstract number: B239
Session Information
Session Name: Poster Session B: Lung Transplantation Poster Session
Session Type: Poster Session
Date: Sunday, April 30, 2017
Session Time: 6:00pm-7:00pm
 Presentation Time: 6:00pm-7:00pm
Presentation Time: 6:00pm-7:00pm
Location: Hall D1
Studies show that insurance status at the time of wait-listing affects waitlist and posttransplant survival after lung transplant. No studies have analyzed the effect of more remote insurance status. We aimed to identify differences in waitlist and posttransplant survival for lung transplant candidates with cystic fibrosis (CF) by insurance status in the 2 years before listing and transplant, respectively.
We merged the Scientific Registry of Transplant Recipients (SRTR) and Cystic Fibrosis Foundation Patient Registry (CFFPR) to create a novel database to describe characteristics of CF patients before listing that may contribute to waitlist and posttransplant mortality. Our cohort includedcandidates aged [sup3]12 years who were listed or underwent transplant 2006-2014.
We performed univariate Kaplan-Meier survival analyses to detect differences in waitlist and posttransplant survival by insurance status (public, private, unknown). Insurancestatus 2 years before listing and transplant, respectively, was obtained from the CFFPR. Waitlist deathorremovalduetoillness and posttransplant survivalwereobtainedfromSRTR.
We identified 2225 candidateswith CF. During the 2 years before listing, 1340 (60%) hadprivate and 633 (28%) hadpublic insurance. One-year waitlist survival was similar in the two groups (78% vs. 76%, log rank P = 0.359). Among 1853 transplant recipients, 1137 (61%) had private and 527 (28%) had public insurance in the 2 years before transplant. One-year posttransplant survival was similar (89% vs. 86%, P = 0.115), but by 2 years, survival was better for those with private insurance (80% vs. 72%, P <0.0001).
CF patient type of insurance did not affect waitlist or 1-year posttransplant survival; however, risk of mortality was increased at 2 years for patients with public insurance. If these findings are confirmed after adjusting for known factors associated with holding public insurance, further research is needed to determine the causes and points of intervention to improve survival in CF patients with public health insurance.
Figure 1: Two-Year Posttransplant Mortality by Insurance Status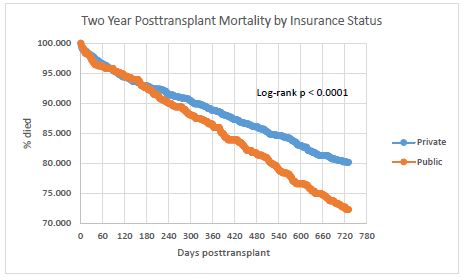
CITATION INFORMATION: Lehr C, Skeans M, Dasenbrook E, Valapour M. The Impact of Insurance Status on Waiting List and Post-Lung Transplant Survival in Patients with Cystic Fibrosis. Am J Transplant. 2017;17 (suppl 3).
To cite this abstract in AMA style:
Lehr C, Skeans M, Dasenbrook E, Valapour M. The Impact of Insurance Status on Waiting List and Post-Lung Transplant Survival in Patients with Cystic Fibrosis. [abstract]. Am J Transplant. 2017; 17 (suppl 3). https://atcmeetingabstracts.com/abstract/the-impact-of-insurance-status-on-waiting-list-and-post-lung-transplant-survival-in-patients-with-cystic-fibrosis/. Accessed February 20, 2026.« Back to 2017 American Transplant Congress
