The Clinical Relevance of cPRA in 0-ABDRDQ Mismatched Kidney Transplants
1Medicine, Division of Nephrology, University of British Columbia, Vancouver, BC, Canada, 2Pathology, Emory University, Atlanta, GA
Meeting: 2020 American Transplant Congress
Abstract number: C-090
Keywords: Highly-sensitized, Histocompatibility, HLA matching, Outcome
Session Information
Session Name: Poster Session C: Kidney Complications: Immune Mediated Late Graft Failure
Session Type: Poster Session
Date: Saturday, May 30, 2020
Session Time: 3:15pm-4:00pm
 Presentation Time: 3:30pm-4:00pm
Presentation Time: 3:30pm-4:00pm
Location: Virtual
*Purpose: The clinical relevance of immune sensitization as measured by cPRA in kidney transplantation remains uncertain.
*Methods: We identified 4,057 adult, first, kidney only transplant recipients from USRDS (2010-2014) who were zero-mismatched with their donors at 4 major HLA loci (HLA-A, -B, -DR, -DQ) and determined outcomes in patient subgroups defined by their pre-transplant cPRA (0% ,n = 1,583; 1-29%, n = 425; 30-79%, n = 847; 80-97%, n = 621; >= 98%, n = 581).
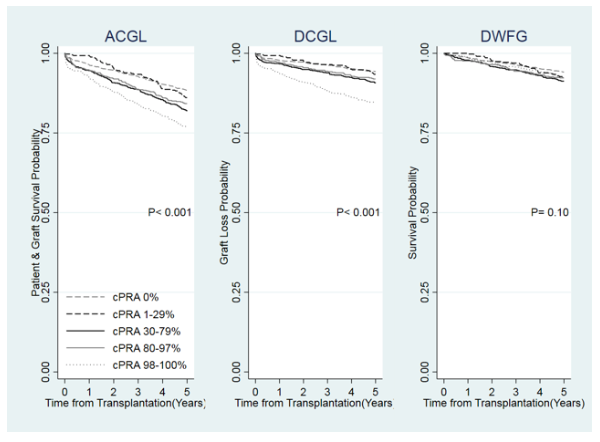
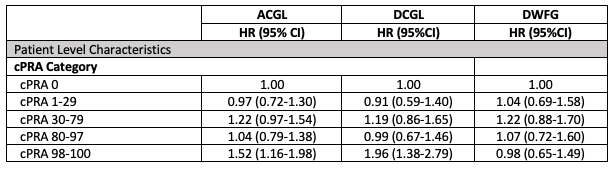
*Results: The Figure shows that the time to graft loss from any cause including death (ACGL) and death censored graft loss (DCGL), but not death with a functioning graft (DWFG), was shorter in patients with higher cPRA. The Table shows the results of separate Cox multivariate regression analyses for the outcomes of ACGL, DCGL and DWFG. The models were adjusted for differences in recipient age, sex, race, cause of ESRD, pre-transplant dialysis vintage, insurance, donor source, donor KDPI, and type of antibody induction.
*Conclusions: There is a higher risk of ACGL and DCGL but not DWFG among 0-ABDRDQ mismatched patients with cPRA >= 98%. The higher risk of transplant failure in these patients may be due to the presence of antibodies at HLA-C and -DP loci, allele-specific antibodies, non-HLA antibodies, or unknown residual confounders. cPRA may not portend increased risk in patients with cPRA < 98%.
To cite this abstract in AMA style:
Lan JH, Chang D, Kadatz M, Gill J, Gebel HM, Gill JS. The Clinical Relevance of cPRA in 0-ABDRDQ Mismatched Kidney Transplants [abstract]. Am J Transplant. 2020; 20 (suppl 3). https://atcmeetingabstracts.com/abstract/the-clinical-relevance-of-cpra-in-0-abdrdq-mismatched-kidney-transplants/. Accessed February 19, 2026.« Back to 2020 American Transplant Congress