The Associations Between Immunosuppression Use, Loss of Medicare and Kidney Allograft Outcomes.
1Hennepin County Medical Center, Minneapolis
2Scientific Registry of Transplant Recipients, Minneapolis
Meeting: 2017 American Transplant Congress
Abstract number: D89
Keywords: Graft failure, Immunosuppression, Kidney, Medicare
Session Information
Session Name: Poster Session D: Kidney Immunosuppression: Novel Regimens and Drug Minimization
Session Type: Poster Session
Date: Tuesday, May 2, 2017
Session Time: 6:00pm-7:00pm
 Presentation Time: 6:00pm-7:00pm
Presentation Time: 6:00pm-7:00pm
Location: Hall D1
Medicare coverage for kidney transplant recipients aged <65 years in the US ends 3 years posttransplant, but a significant proportion of recipients remain on Medicare under disability coverage. We sought to describe the association of immunosuppressant use and loss of Medicare with subsequent graft failure.
We linked the Medicare payer sequence file (January 1, 2008-December 31, 2014) and the IMS Health pharmacy fills database (January 1, 2001-October 1, 2012) with data from the Scientific Registry for Transplant Recipients. Immunosuppressant use was defined as a medication possession ratio (MPR), calculated as the sum of days supplied divided by days at risk for filling. The retrospective cohort included Medicare-covered adult kidney-alone transplant recipients, January 1, 2008-December 31, 2009, with graft function at 2.5 years posttransplant who filled at least one immunosuppressant in IMS 2 to 2.5 years posttransplant (n = 7334). A Cox proportional hazards model was used to evaluate the association between class-specific MPRs over 6-month time intervals and time-dependent loss of Medicare on allograft failure after 2.5 years posttransplant.
Loss of Medicare was associated with lower risk of graft failure in unadjusted analysis (HR 0.83, 95% CI 0.71-0.96), but the relationship became nonsignificant after adjusting for donor and recipient factors. Use of calcineurin inhibitors (CNIs) and antimetabolites declined slightly but significantly after loss of Medicare. Conversely, the associations of lower CNI and antimetabolite use with graft failure remained significant after adjustment (HR 0.83, 95% CI 0.70-0.98; 0.58, 95% CI 0.48-0.70, respectively).
Lower CNI and antimetabolite use was associated with higher risk of graft failure. However, we could not detect an association between loss of Medicare coverage and higher risk of graft failure after adjusting for immunosuppression use, donor type, and recipient health measures. This association should be evaluated in the general kidney transplant population, as our cohort size was small due to the limited amount of pharmacy fill data.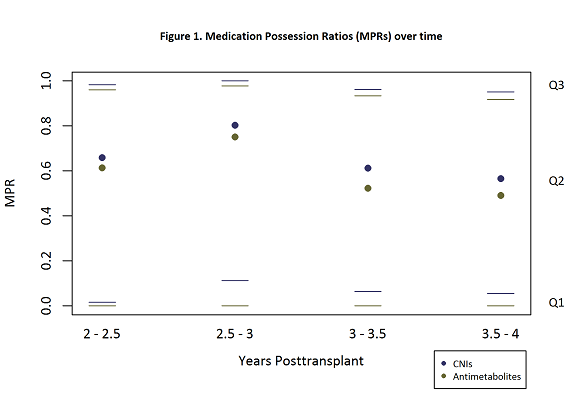
CITATION INFORMATION: Hart A, Gustafson S, Wey A, Hadley N, Israni A. The Associations Between Immunosuppression Use, Loss of Medicare and Kidney Allograft Outcomes. Am J Transplant. 2017;17 (suppl 3).
To cite this abstract in AMA style:
Hart A, Gustafson S, Wey A, Hadley N, Israni A. The Associations Between Immunosuppression Use, Loss of Medicare and Kidney Allograft Outcomes. [abstract]. Am J Transplant. 2017; 17 (suppl 3). https://atcmeetingabstracts.com/abstract/the-associations-between-immunosuppression-use-loss-of-medicare-and-kidney-allograft-outcomes/. Accessed February 18, 2026.« Back to 2017 American Transplant Congress
