The Acuity Circle Allocation Policy is Associated with Worse Graft Survival After Liver Transplant with Donation After Circulatory Death Donors in Low-MELD Centers
T. Kitajima1, T. Ivanics2, D. Moonka1, M. Shamaa1, A. Mohamed3, S. Shimada1, K. Collins4, M. Rizzari1, A. Yoshida1, M. Abouljoud4, S. Nagai1
1Henry Ford Hospital, Detroit, MI, 2Surgery, Henry Ford Hospital, Detroit, MI, 3Department of Transplant and Hepatobiliary Surgery, Henry Ford Hospital, Detroit, MI, 4Henry Ford Transplant Institute, Detroit, MI
Meeting: 2022 American Transplant Congress
Abstract number: 226
Keywords: Allocation, Donors, non-heart-beating, Liver transplantation, Survival
Topic: Clinical Science » Liver » 59 - Liver: Expanding the Donor Pool* (Liver: MELD Allocation / Donor Issues)
Session Information
Session Name: Expanding the Donor Pool (MELD Allocation/Donor Issues)
Session Type: Rapid Fire Oral Abstract
Date: Monday, June 6, 2022
Session Time: 3:30pm-5:00pm
 Presentation Time: 3:40pm-3:50pm
Presentation Time: 3:40pm-3:50pm
Location: Hynes Room 312
*Purpose: Liver allocation in the United States was updated in February of 2020, with introduction of the acuity circle (AC) model. However, the effect of AC model on liver transplant (LT) outcomes using donation after circulatory death (DCD) donor grafts has not been investigated. This study aims to analyze the early effects of AC-based allocation on post-LT outcomes in DCD-LT.
*Methods: Using OPTN/UNOS data, we analyzed adult LT recipients between Jan 1, 2018 and Sep 30, 2020 excluding LDLT and multi-organ transplant. Median MELD score at each transplant center was calculated and centers were categorized as low- (<25%ile, n=37), mid- (25-75%ile, n=80) or high-MELD (>75%ile, n=25) centers. Two eras were defined by the LT date (pre- and post-AC) and DCD utility was compared in each center group. In DCD-LTs, 180-day/1-year graft survival (GS) were compared. Risks for graft loss (GL) were analyzed using Cox proportional hazard model, with risk adjustments for recipient and donor variables.
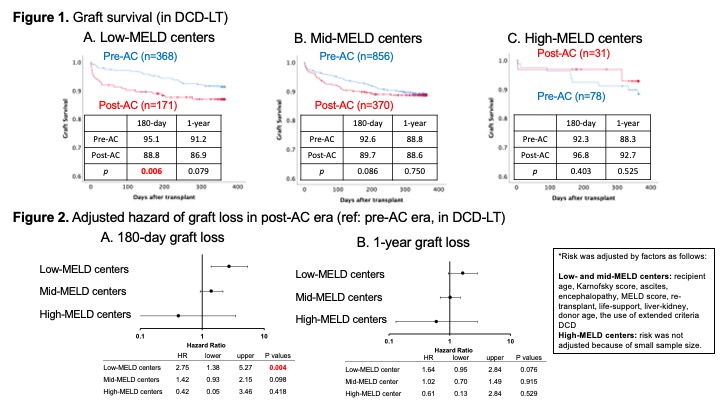
*Results: There were 19,088 DBD and 1,874 DCD-LT recipients. The proportion of DCD-LT was higher in post-AC than in pre-AC era in low-MELD (16.8% vs 11.4%, P<0.001) and mid-MELD centers (10.9% vs 8.3%, P<0.001). In DCD-LTs, recipient age and MELD score were similar between eras in all center groups, and donor age, cold ischemia time, and distance from donor hospital were similar in low- and high-MELD centers. The post-AC era was associated with an increased risk of 180-day GL (ref: pre-AC, HR 1.64, 95% CI 1.15-2.33; p=0.006). In low-MELD centers, DCD-LTs in the post-AC era had a lower 180-day GS (post-AC 88.8% vs. pre-AC 95.1%, p=0.006, Figure 1). After risk adjustment, in low-MELD centers, post-AC era was associated with a higher risk-adjusted hazard of 180-day GL (ref: pre-AC, HR 2.75, 95% CI 1.38-5.27; p=0.004). In contrast, the post-AC era was not associated with a higher risk of GL in mid-MELD and high-MELD centers (Figure 2).
*Conclusions: The use of DCD donors in low- and mid-MELD centers was higher after the implementation of the AC policy. Moreover, the post-AC era was associated with an increased risk of graft loss only in low-MELD centers. The regional disparity in DCD use and outcomes in the early post-AC period warrants close monitoring to inform future allocation policy refinements.
To cite this abstract in AMA style:
Kitajima T, Ivanics T, Moonka D, Shamaa M, Mohamed A, Shimada S, Collins K, Rizzari M, Yoshida A, Abouljoud M, Nagai S. The Acuity Circle Allocation Policy is Associated with Worse Graft Survival After Liver Transplant with Donation After Circulatory Death Donors in Low-MELD Centers [abstract]. Am J Transplant. 2022; 22 (suppl 3). https://atcmeetingabstracts.com/abstract/the-acuity-circle-allocation-policy-is-associated-with-worse-graft-survival-after-liver-transplant-with-donation-after-circulatory-death-donors-in-low-meld-centers/. Accessed March 3, 2026.« Back to 2022 American Transplant Congress