Temporal Changes in Renal Function Predict Waitlist Death or Deterioration in Pediatric Liver Transplantation
Mayo Clinic Rochester, Minnesota, Rochester, MN
Meeting: 2021 American Transplant Congress
Abstract number: 1177
Keywords: Liver transplantation, Pediatric, Renal dysfunction, Waiting lists
Topic: Clinical Science » Liver » Liver: Pediatrics
Session Information
Session Name: Liver: Pediatrics
Session Type: Poster Abstract
Session Date & Time: None. Available on demand.
Location: Virtual
*Purpose: Renal dysfunction at the time of listing predicts inferior waitlist outcomes in pediatric liver transplant candidates, independent of the Pediatric End-Stage Liver Disease (PELD) score. We test the hypothesis that temporal changes in post-transplant listing renal function also impact waitlist death or deterioration.
*Methods: We studied all pediatric patients <12 years old registered for liver-only transplantation in the United States between Feb 2002-Dec 2018. Status 1A listings were excluded. Patients were stratified into categories of high (eGFR≥90mL/min/1.73m2), intermediate (eGFR 60-89 mL/min/1.73m2) or low eGFR (eGFR<60mL/min/1.73m2 or on dialysis) at transplant registration. Multivariable logistic regression models were used to assess the impact of improving and worsening eGFR on 90-day waitlist death/deterioration.
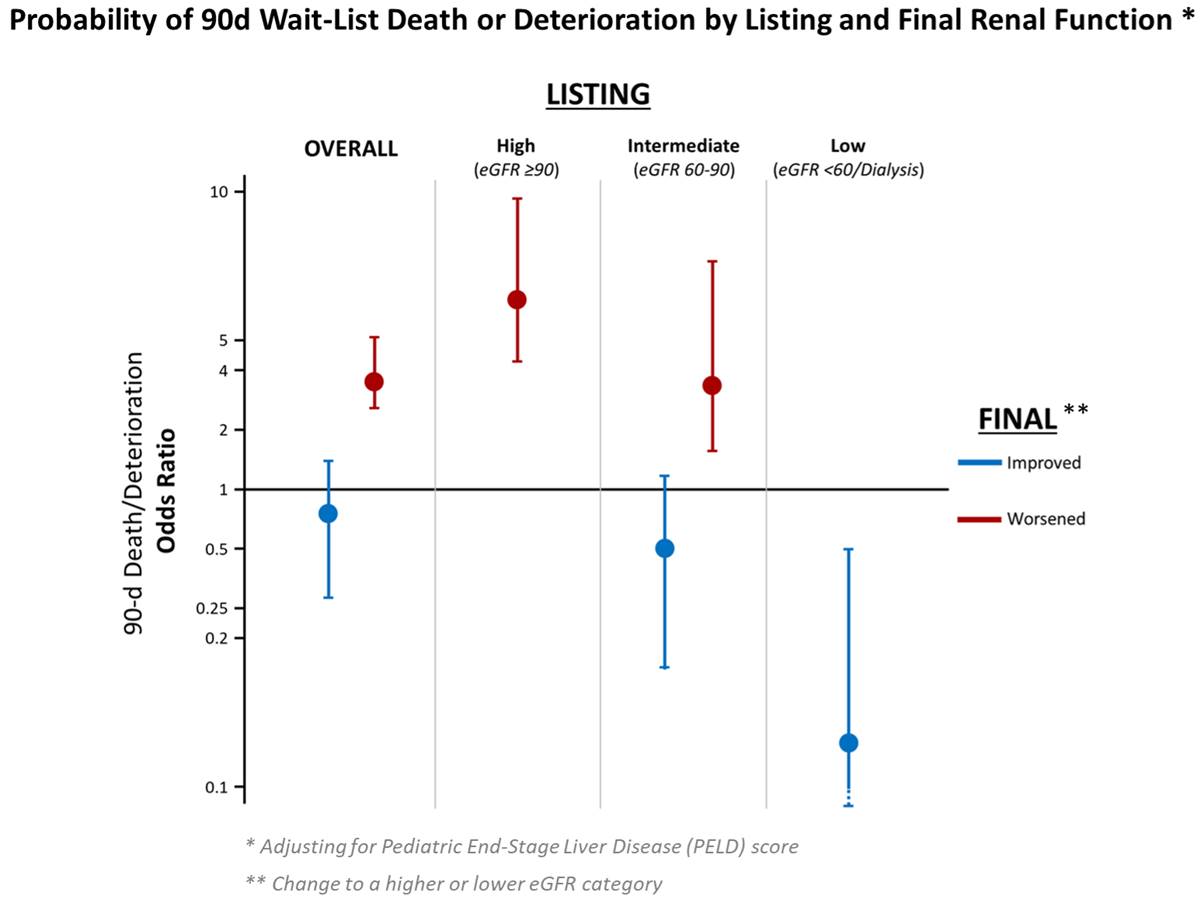
*Results: A total of 4,578 patients met study criteria. Median (inter-quartile) age was 1 (0-3) year, and 50% (2,267) were male. Overall, 80% (3,654) of patients proceeded to transplant, and 6.5% (298) died or deteriorated beyond transplantability. At listing, 80.5% (3,553) had high eGFR, 14.6% (644) had intermediate eGFR, and 4.9% (217) had low eGFR. At waitlist removal, renal function had improved to a higher eGFR category in 7.1% (315) of patients, and 14.9% (658) had worsening of renal function to a lower eGFR category, compared to listing measurements. Adjusting for PELD score, odds of 90-day waitlist death/deterioration markedly increased in patients with worsening eGFR versus those in whom it was unchanged (OR 3.71, 95%CI 2.67-5.16; p<0.001). This was clear in subsets with high (OR 6.41, 95%CI 4.24-9.66) or intermediate eGFR (OR 3.51, 95%CI 1.60-7.69) at transplant listing (both p<0.001). Though a trend toward favorable 90-day outcomes in patients with improved eGFR did not reach significance for the overall cohort, in those with the lowest category eGFR at listing, improvements in renal function were associated with an 8-fold reduction in odds of 90-day death/deterioration (OR 0.13, 95%CI 0.04-0.48; p=0.002). (Figure)
*Conclusions: Worsening waitlist renal function independently predicts 90-day death/deterioration in pediatric liver transplant candidates. In those with the lowest eGFR at registration, temporal improvements in renal function were associated with favorable outcome. These data highlight prognostic merits of aggressively managing waitlist kidney dysfunction, while further supporting integration of renal function parameters in the process of liver allocation to pediatric transplant candidates.
To cite this abstract in AMA style:
Thalji N, Thalji L, Ibrahim S, Diwan T, Kamath P, Heimbach J. Temporal Changes in Renal Function Predict Waitlist Death or Deterioration in Pediatric Liver Transplantation [abstract]. Am J Transplant. 2021; 21 (suppl 3). https://atcmeetingabstracts.com/abstract/temporal-changes-in-renal-function-predict-waitlist-death-or-deterioration-in-pediatric-liver-transplantation/. Accessed February 18, 2026.« Back to 2021 American Transplant Congress