Taking a Step toward Standardization: Results of an American Society of Transplant Surgeons/Association of Organ Procurement Organizations Survey of Donation after Circulatory Death Liver Recovery Practices
1American Society of Transplant Surgeons DCD Task Force, Arlington, VA, 2Association of Organ Procurement Organizations, Vienna, VA
Meeting: 2019 American Transplant Congress
Abstract number: C289
Keywords: Cadaveric organs, Donors, non-heart-beating, Liver transplantation, Procurement
Session Information
Session Name: Poster Session C: Liver: MELD, Allocation and Donor Issues (DCD/ECD)
Session Type: Poster Session
Date: Monday, June 3, 2019
Session Time: 6:00pm-7:00pm
 Presentation Time: 6:00pm-7:00pm
Presentation Time: 6:00pm-7:00pm
Location: Hall C & D
*Purpose: Donation after circulatory death (DCD) liver transplants (LT) represented only 6.3% of total U.S. LT in 2017, despite DCD comprising 18.3% of the deceased donor pool. Non-standardization of donation after circulatory death (DCD) procurement practices at both the transplant center and organ procurement organization (OPO) level may contribute to DCD LT under-utilization. In order to develop uniform DCD recovery standards, current variations in transplant surgeon and OPO DCD recovery practices must be better defined.
*Methods: Transplant surgeon surveys were distributed electronically to ASTS members, and OPO surveys were distributed electronically by AOPO.
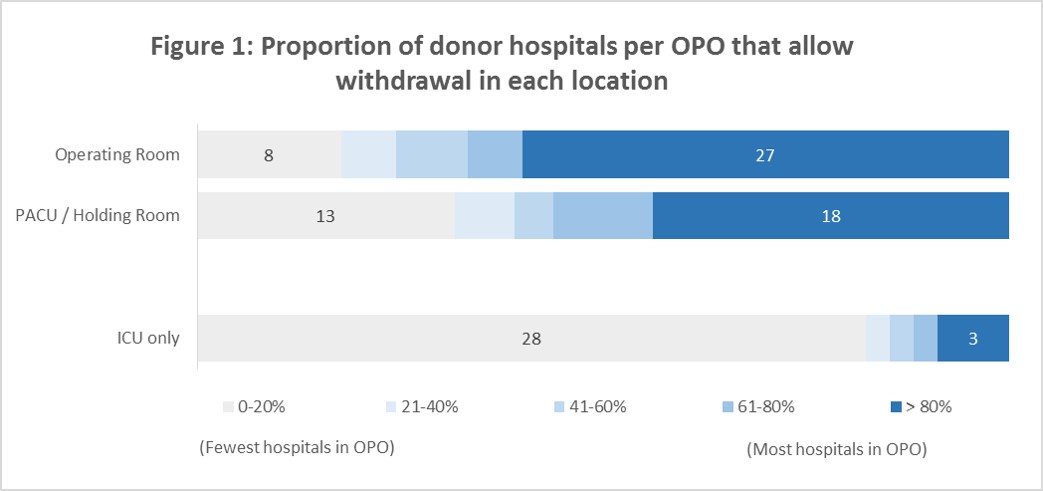
*Results: 188 transplant surgeons and 48 OPOs responded. 72.4% of surgeons responded that attending surgeon DCD liver recovery is necessary, while only 27.7% of OPOs share this requirement. Pre-withdrawal communication huddle (Surgeons: 88.7%; OPOs: 93.75%) and administration of pre-withdrawal heparin (Surgeons: 90.57%; OPOs: 84.8%) are widely accepted by both stakeholder groups. Although 89.31% of surgeons prefer OR withdrawal of support when recovering a DCD liver, OPO practice varies widely. (Figure 1) Most surgeons and OPOs consider aortic flush, not aortic cross-clamping, to define the end of donor warm ischemia time (dWIT) (Surgeons: 81.76%; OPOs: 81.25%). However, surgeons and OPOs have very different intra- and inter- group definitions of the start of dWIT. 50% of surgeons consider withdrawal of support to be the beginning of dWIT, with the remainder using a hemodynamic/oxygenation parameter. 87.2% of OPOs use oxygen saturation <80 and 76% use systolic blood pressure <80 to define start of dWIT.
*Conclusions: Some DCD liver recovery practices have broad surgeon and OPO consensus, including mandatory communication huddle, pre-withdrawal heparin administration, and end of dWIT. These broadly-accepted practices should be considered standard-of-care and implemented into hospital-based DCD policies. There is no consensus between surgeons and OPOs on several critical organ recovery details, including location of withdrawal of support and the definition of the start of dWIT. Resolving these discrepancies and creating a complete set of national DCD recovery standards is an important next step towards improving DCD liver utilization.
To cite this abstract in AMA style:
Hobeika M, Glazner R, Foley D, Hanish S, Quintini C, Eidbo E, Axelrod D. Taking a Step toward Standardization: Results of an American Society of Transplant Surgeons/Association of Organ Procurement Organizations Survey of Donation after Circulatory Death Liver Recovery Practices [abstract]. Am J Transplant. 2019; 19 (suppl 3). https://atcmeetingabstracts.com/abstract/taking-a-step-toward-standardization-results-of-an-american-society-of-transplant-surgeons-association-of-organ-procurement-organizations-survey-of-donation-after-circulatory-death-liver-recovery-pra/. Accessed March 2, 2026.« Back to 2019 American Transplant Congress