T cell Phenotypes Predict Infectious Risk in Transplanted Children
1Pediatrics/Surgery, Duke University, Durham
2Pediatrics, UCLA, Los Angeles
3Pediatrics, Emory, Atlanta
4Pediatrics, Stanford, Palo Alto
5Surgery, UCSF, San Francisco.
Meeting: 2018 American Transplant Congress
Abstract number: 601
Keywords: Kidney transplantation, Lymphocytes, Pediatric
Session Information
Session Name: Concurrent Session: Late Breaking
Session Type: Concurrent Session
Date: Tuesday, June 5, 2018
Session Time: 4:30pm-6:00pm
 Presentation Time: 5:06pm-5:18pm
Presentation Time: 5:06pm-5:18pm
Location: Room 3AB
AIM: Current monitoring strategies do not adequately differentiate infection from complications such as allograft rejection (AR). We aimed to identify peripheral T cell phenotypes that could predict and differentiate infection from AR in pediatric renal transplantation.
Methods: 104 children (age 1-21) from the multi-center, NIH funded, Immune Development in Pediatric Transplantation (IMPACT) study were prospectively followed for 1 year post-kidney transplantation. Patients were categorized by having no event, protective immune failure, defined as viremia by quantitative PCR for BK, EBV, CMV, Adenovirus, Human Herpesvirus, or JC virus and/or clinical infection, or alloimmune failure, defined as biopsy proven AR and/or presence of donor specific antibody (DSA). Multiparameter flow cytometry for naive CD45RA+CCR7+, central memory CD45RA-CCR7+, effector memory CD45RA-CCR7-, effector memory RA CD45RA+CCR7- , senescent (CD57+) and exhausted (PD1+) T cell populations were monitored.
Results: Of 104 patients, 16 (15.4%) had no event, 66 (63.5%) had impaired protective immunity, 22 (22.1%) had alloimmune failure. For patients with impaired protective immunity, viremia occurred in 97% (64/66) and associated clinical viral and bacterial infections had a frequency of 34.8% (23/66) and 18.2% (12/66). The median time to impaired protective immunity was 111.5 days (IQR 47.8-209.8) compared to 29.5 days (IQR 16.2-159.8) for alloimmune failure. Significant changes with higher naive CD4 T cells (Figure 1A), lower CD4 effector memory cells (Figure 1B) and lower CD4 PD-CD57+ T cells (Figure 1C) were seen in patients with impaired protective immunity prior to and persisting after the infection compared to no event or alloimmune failure. 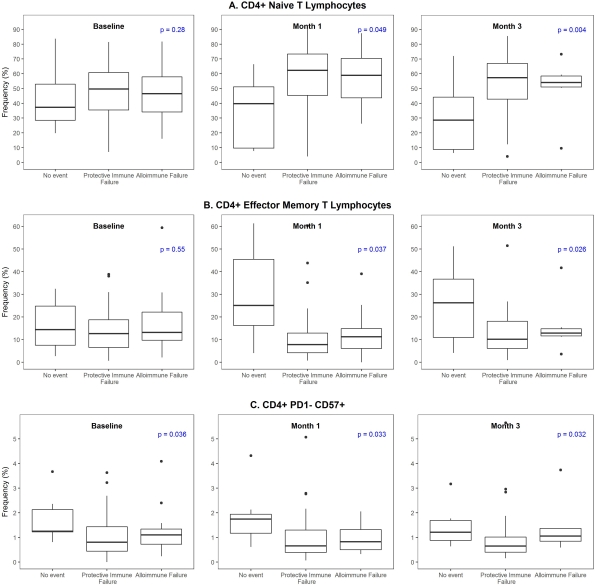
Conclusions: We have identified a CD4 T cell signature that can potentially predict/monitor patients at risk for infection, leading to medication optimization and decreased infectious related morbidity.
CITATION INFORMATION: Chambers E. T., Ettenger R., Lee H.-J., Chan C., Stempora L., Warshaw B., Grimm P., Reed E. F., Sarwal M., Kirk A. T cell Phenotypes Predict Infectious Risk in Transplanted Children Am J Transplant. 2017;17 (suppl 3).
To cite this abstract in AMA style:
Chambers ET, Ettenger R, Lee H-J, Chan C, Stempora L, Warshaw B, Grimm P, Reed EF, Sarwal M, Kirk A. T cell Phenotypes Predict Infectious Risk in Transplanted Children [abstract]. https://atcmeetingabstracts.com/abstract/t-cell-phenotypes-predict-infectious-risk-in-transplanted-children/. Accessed February 21, 2026.« Back to 2018 American Transplant Congress
