Survival Benefit of Simultaneous Liver Kidney (SLK) Transplant in Liver Transplant Candidates With Renal Dysfunction
1Medicine/Nephrology, UT Southwestern, Dallas, TX
2Clinical Sciences, UT Southwestern, Dallas, TX
3Medicine/Hepatology, UT Southwestern, Dallas, TX.
Meeting: 2015 American Transplant Congress
Abstract number: B135
Keywords: Kidney/liver transplantation, Liver cirrhosis, Mortality, Renal dysfunction
Session Information
Session Name: Poster Session B: Liver - Kidney Issues in Liver Transplantation
Session Type: Poster Session
Date: Sunday, May 3, 2015
Session Time: 5:30pm-6:30pm
 Presentation Time: 5:30pm-6:30pm
Presentation Time: 5:30pm-6:30pm
Location: Exhibit Hall E
Survival benefit of SLK over liver transplant alone (LTA) in patients with same level of renal dysfunction and effect of organ quality on mortality are not well studied.
We analyzed OPTN registry that included adult LTA and SLK recipients transplanted between 2002 and 2013. Primary outcomes were post-transplant mortality and effect of donor quality on post-transplant mortality. We excluded patients with Status 1 and the ones who received exception MELD points. The study cohort (N=4,729) was divided into 4 groups based on renal function at listing and transplant: LK1: not on dialysis at listing and serum creatinine (Scr) <2 mg/dl at transplant; LK2: not on dialysis at listing and Scr≥2 mg/dl at transplant; LK3: not on dialysis at listing but on dialysis at transplant; LK4: on dialysis at listing and transplant. Since liver transplant recipients with renal dysfunction were not randomly assigned to LTA vs. SLK, selection bias was adjusted for by developing a propensity score (PS) matching. We constructed a propensity score based on a model that is stratified by transplant type in 4 different groups (LTA vs. SLK in LK1, LK2, LK3, and LK4). The variables were used in the propensity score as follows: age, gender, race, BMI, recipient diabetes, underlying liver disease etiology, Scr at transplant, serum bilirubin at transplant, INR at transplant, wait list duration, and liver donor risk index (DRI) score.
Results are shown below on the table and figure.
SLK offers survival benefit in patients with LK2 (pre-transplant chronic renal dysfunction Scr>2mg/dl but not exposed to dialysis). Mortality rate significantly differs with donor quality. Decrease in mortality risk for SLK was restricted to better quality donors (liver DRI scores<1.3 or equivalent kidney donor profile index –KDPI<40%).
| HR | 95%CI | P | |
| LK1 | 0.75 | 0.50-1.12 | 0.155 |
| LK2 | 0.78 | 0.63-0.96 | 0.021 |
| LK3 | 0.84 | 0.68-1.04 | 0.106 |
| LK4 | 0.83 | 0.65-1.05 | 0.122 |
Effect of liver DRI on mortality in SLK compared with LTA.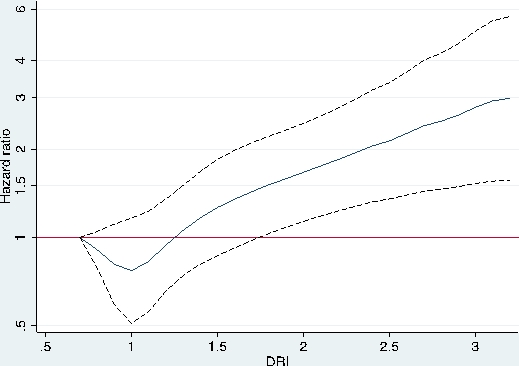
To cite this abstract in AMA style:
Tanriover B, Zhang S, Marrero J. Survival Benefit of Simultaneous Liver Kidney (SLK) Transplant in Liver Transplant Candidates With Renal Dysfunction [abstract]. Am J Transplant. 2015; 15 (suppl 3). https://atcmeetingabstracts.com/abstract/survival-benefit-of-simultaneous-liver-kidney-slk-transplant-in-liver-transplant-candidates-with-renal-dysfunction/. Accessed July 18, 2025.« Back to 2015 American Transplant Congress
