Survival Benefit of Partial Grafts in Pediatric Candidates with Acute Liver Failure Awaiting Liver Transplantation: SRTR Analysis over 26 Years
D. Firl, K. Sasaki, C. Quintini, B. Eghtesad, C. Miller, K. Hashimoto.
CCF, Cleveland.
Meeting: 2018 American Transplant Congress
Abstract number: 359
Keywords: Infant, Liver transplantation, Living-related liver donors, Pediatric
Session Information
Session Name: Concurrent Session: Liver: Pediatrics
Session Type: Concurrent Session
Date: Monday, June 4, 2018
Session Time: 4:30pm-6:00pm
 Presentation Time: 4:42pm-4:54pm
Presentation Time: 4:42pm-4:54pm
Location: Room 608/609
Objective: Pediatric fulminant hepatic failure (PFHF) is a devastating condition which portends a poor prognosis without liver transplantation (LT). In comparison to adult candidates, there are fewer suitable donor organs from deceased donors (DDLT); this study was conducted to estimate the utility of partial liver grafts (split/reduced [SRLT] and live donors [LDLT]).
Methods: This study used the scientific registry of transplant recipients (SRTR) from 1995-2015, evaluating primary and secondary diagnoses for: acute hepatic necrosis, acute viral hepatitis, toxic insult, and unknown fulminant failure (n= 2419 candidates). Candidate status was evaluated using SRTR delisting codes (n for LT=1339, recovered=632, died=364) and post-LT followup (mean 76.9 months). Cox proportional hazards models using competing risks and the Kaplan-Meier method assessed prognostic outcomes.
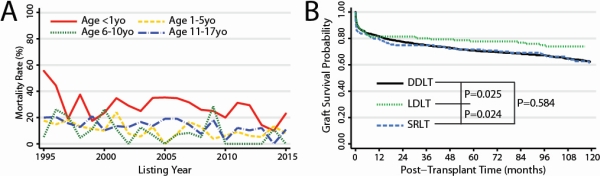
Results: From 1995-2015, there was a significant decrease from ~150 to ~75 PFHF per year (P<0.0001). Although waitlist mortality is overall decreasing (19.1% to 9.7%) and successful transplantations increased (53.7% to 62.2%) (Figure 1A, P<0.0001), patients in the <1yo group had persistently high mortality (>20%) compared to the other age groups (P<0.0001). Partial grafts, those most likely to fit pediatric candidates, are underutilized (25.7% of cases). In the adjusted model, amongst other factors, increased age [HR=0.95 per year; P=0.004] and access to partial grafts was significantly associated with decreased risk of waiting list mortality [HR=0.67; P=0.040]. LDLT recipients had shorter median waiting times compared to deceased donors (3 days-LDLT vs 4-DDLT vs 5-SRLT; P=0.017). Patients receiving partial grafts had similar 5-year graft survival compared to whole DDLT (Figure 1B, 78.3% for LDLT, 70.9% for DDLT, 72.1% for SRLT).
Conclusions: PFHF patients <1yo remain disadvantaged due to difficulty with finding a suitable donor organ. In these patients, listing at centers with experienced partial graft programs improved outcomes (both pre- and post-LT). Partial grafts should be sought early, not delayed in hopes of a suitable deceased donor.
CITATION INFORMATION: Firl D., Sasaki K., Quintini C., Eghtesad B., Miller C., Hashimoto K. Survival Benefit of Partial Grafts in Pediatric Candidates with Acute Liver Failure Awaiting Liver Transplantation: SRTR Analysis over 26 Years Am J Transplant. 2017;17 (suppl 3).
To cite this abstract in AMA style:
Firl D, Sasaki K, Quintini C, Eghtesad B, Miller C, Hashimoto K. Survival Benefit of Partial Grafts in Pediatric Candidates with Acute Liver Failure Awaiting Liver Transplantation: SRTR Analysis over 26 Years [abstract]. https://atcmeetingabstracts.com/abstract/survival-benefit-of-partial-grafts-in-pediatric-candidates-with-acute-liver-failure-awaiting-liver-transplantation-srtr-analysis-over-26-years/. Accessed February 17, 2026.« Back to 2018 American Transplant Congress