Survival Benefit of Liver Transplant Among HIV+ Waitlist Candidates
C. Durand,1 S. Gustafson,2 J. Locke,3 J. Snyder,2 B. Shelton,3 R. Reed,3 P. MacLennan,3 S. Mehta,3 A. Nellore,3 D. Segev.1,2
1Johns Hopkins University, Baltimore, MD
2Scientific Registry of Transplant Recipients (SRTR), CDRG, Minneapolis, MN
3University of Alabama, Birmingham, Birmingham, Al.
Meeting: 2015 American Transplant Congress
Abstract number: D269
Keywords: HIV virus, Liver transplantation, Survival, Waiting lists
Session Information
Session Name: Poster Session D: Viral Infections
Session Type: Poster Session
Date: Tuesday, May 5, 2015
Session Time: 5:30pm-6:30pm
 Presentation Time: 5:30pm-6:30pm
Presentation Time: 5:30pm-6:30pm
Location: Exhibit Hall E
Liver failure is the most common cause of non-AIDS related death among HIV+ patients, primarily due to high prevalence of co-infection with hepatitis C (HCV) and hepatitis B (HBV) virus. Recent prospective clinical trials have demonstrated good outcomes of liver transplantation (LT) in select HIV/HCV co-infected patients with end-stage liver disease (ESLD). However, no study has examined LT recipient survival vs. survival of all HIV+ ESLD patients on the LT waiting list. IMS pharmacy fills (1/1/01-10/1/12) were linked with SRTR data. LT waitlist candidates who filled >1 antiretroviral (ARV) medication unique to HIV treatment were identified and followed from the later of date of listing or first known HIV medication fill; simultaneous listings were collapsed. Time to event (waitlisting to death or administrative end of study) survival analyses were performed using Cox proportional hazard modeling, adjusted for available waitlist covariates. Number of transplants was treated as a time-dependent categorical variable (0, 1, 2). Of 437 HIV+ LT waitlist candidates, 93% filled >1 ARV and 31% had a primary diagnosis other than HCV or HBV. First-time LT was associated with a 68% lower risk of death vs. no transplant (adjusted hazard ratio [AHR] 0.32, 95%CI 0.22-0.46, p<0.0001); AHR for second LT suggested reduced mortality risk, but was not statistically significant (0.30, 0.08-1.1, p=0.07]. Lack of significance may be due to sample size (n=12 repeat vs. n=199 first LTs). In a large cohort of HIV+ ESLD patients awaiting transplant, survival benefit from LT was significant, not limited to HCV+ or HBV+ recipients, and present for patients with diverse ESLD etiologies. 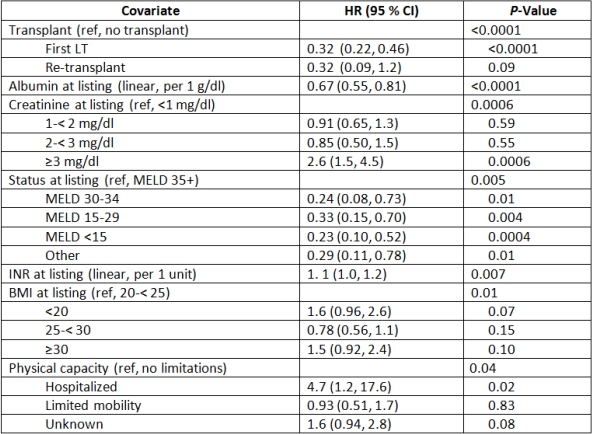
To cite this abstract in AMA style:
Durand C, Gustafson S, Locke J, Snyder J, Shelton B, Reed R, MacLennan P, Mehta S, Nellore A, Segev D. Survival Benefit of Liver Transplant Among HIV+ Waitlist Candidates [abstract]. Am J Transplant. 2015; 15 (suppl 3). https://atcmeetingabstracts.com/abstract/survival-benefit-of-liver-transplant-among-hiv-waitlist-candidates/. Accessed March 6, 2026.« Back to 2015 American Transplant Congress
