Surging Liver Transplant Rates for Alcohol-Associated Liver Disease May Exacerbate Waitlist Death of Patients with Hepatocellular Carcinoma in MMAT-3 Era
1Division of Gastrointestinal and Liver Diseases, University of Southern California, Los Angeles, CA, 2University of Southern California, Los Angeles, CA
Meeting: 2022 American Transplant Congress
Abstract number: 1109
Keywords: Alcohol, Hepatocellular carcinoma, Liver transplantation, Waiting lists
Topic: Clinical Science » Liver » 60 - Liver: MELD Allocation*
Session Information
Session Time: 7:00pm-8:00pm
 Presentation Time: 7:00pm-8:00pm
Presentation Time: 7:00pm-8:00pm
Location: Hynes Halls C & D
*Purpose: Rates of liver transplantation (LT) for alcohol-associated liver disease (ALD) have increased significantly, in part related to broader acceptance of severe alcohol hepatitis (AH) as indication. We hypothesize that greater allocation of organs to ALD, especially those with AH who typically have high MELD-Na, may lead to greater wait time and waitlist mortality for other diagnoses, with particular concern for hepatocellular carcinoma (HCC).
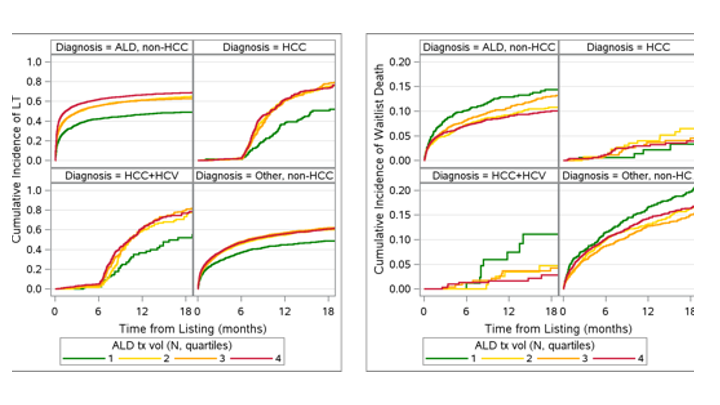
*Methods: Adults (≥18 years) listed for LT from 2014-3/31/2021 in the UNOS database were included. Re-transplant, Status 1, and multi-organ transplants (except kidney) were excluded. Indication for LT was grouped as HCC, HCC+ hepatitis C (HCV), ALD, and Others. Annual center-level ALD transplant volume was assigned to each candidate for their listing year and categorized as quartiles of increasing ALD volume (Q1: <14 to Q4: >36 ALD transplants/year). Cumulative incidence of WL death (died/deteriorated) and LT were estimated and competing-risk regression assessed the association of ALD transplant volume with WL outcomes adjusted for clinical factors.
*Results: 61,403 candidates listed during three UNOS HCC policy eras: pre-6-month-wait (n=12,354), 6-month wait (n=30,773) and MMAT-3 (n=18,273). 1-yr probability of LT for ALD increased from 0.41 in 2014 to 0.63 in 2020, yet declined for HCC from 0.65 in 2014 to 0.60 in 2020. Focusing on the MMAT-3 policy era, of 18,273 listed, 7.1%, 4.2%, 46.4%, and 42.3% were waitlisted for HCC, HCC+HCV, ALD, and Other. Cumulative incidence of LT increased with higher ALD volume [Q2-Q4 vs Q1] for all etiologies. In contrast, waitlist death increased for HCC by higher ALD volume [Q2-Q4 vs Q1] but not for HCC+HCV. The adjusted probability of WL death was 1.5-2-fold higher by ALD volume Q2-Q4 vs Q1 among HCC [sHR Q2=2.1(CI 0.8-5.8), Q3=1.5(CI 0.6-4.0), and Q4=1.5(CI 0.5-4.3)] but lower among ALD [sHR Q2=0.7(CI 0.5-1.0), Q3=0.8(CI 0.6-1.0), and Q4=0.7(CI0.5-0.9)] with a significant interaction for Q2 sHR in HCC vs ALD (p=0.03).
*Conclusions: Early data from the MMAT-3 policy era suggests an association between waitlist death and center-level ALD transplant volume that differs for patients with HCC vs ALD and other etiologies. These data deserve future investigation with longer follow-up to fully understand the impact of shifting LT epidemiology and policy changes.
To cite this abstract in AMA style:
Yuan L, Dodge JL, Zhou K, Terrault N. Surging Liver Transplant Rates for Alcohol-Associated Liver Disease May Exacerbate Waitlist Death of Patients with Hepatocellular Carcinoma in MMAT-3 Era [abstract]. Am J Transplant. 2022; 22 (suppl 3). https://atcmeetingabstracts.com/abstract/surging-liver-transplant-rates-for-alcohol-associated-liver-disease-may-exacerbate-waitlist-death-of-patients-with-hepatocellular-carcinoma-in-mmat-3-era/. Accessed February 19, 2026.« Back to 2022 American Transplant Congress