Social Loafing: Distribution of Kidneys with Multiple Renal Arteries in a National Paired Kidney Exchange Program
G. R. Roll1, W. Irish2, M. Cooper3, M. Ronin4, G. Hil4, A. D. Waterman5, D. B. Leeser2
1UCSF, San Francisco, CA, 2ECU, Greenville, NC, 3Georgetown Univ, Washington, DC, 4NKR, Babylon, NY, 5UCLA and Terasaki Research Institute, Los Angeles, CA
Meeting: 2019 American Transplant Congress
Abstract number: 514
Keywords: Donors, unrelated, Graft survival, High-risk, Kidney transplantation
Session Information
Session Name: Concurrent Session: Kidney Paired Exchange
Session Type: Concurrent Session
Date: Tuesday, June 4, 2019
Session Time: 2:30pm-4:00pm
 Presentation Time: 3:42pm-3:54pm
Presentation Time: 3:42pm-3:54pm
Location: Room 206
*Purpose: To describe the distribution and outcomes after kidney transplantation of multiple renal artery kidneys (MRAK) in a national exchange program.
*Methods: We retrospectively reviewed donor kidney anatomy, distribution of MRAK transplants across participating centers, and patient and graft survival in the National Kidney Registry (NKR) between 2012 and 2017. Survival curves were estimated using the Kaplan-Meier method and compared by the log-rank test. Cumulative incidence function for death-censored graft failure (DCGF) was estimated and compared by Gray’s test. Multivariable Cox’s random-effects model was used to evaluate center variation in the risk of graft failure.
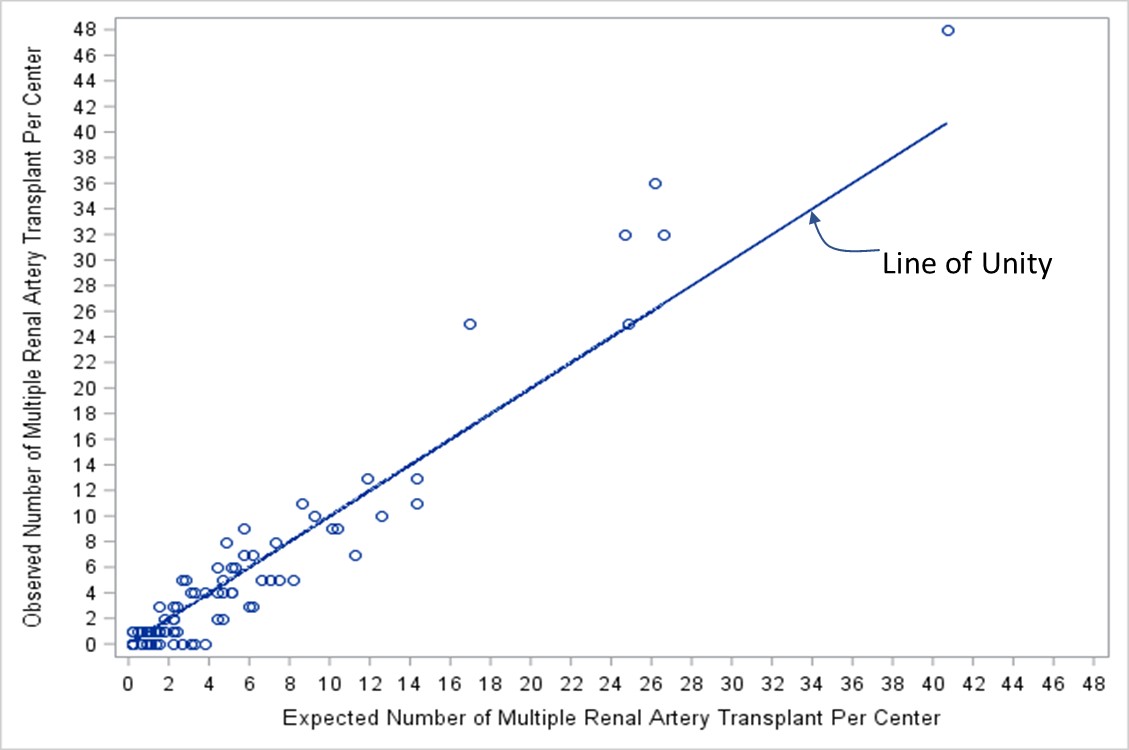
*Results: Of the 2,051 transplants, 451 (22.0%) were MRAK. Plot of the observed to expected number of MRAK transplants per center is provided in Figure 1. Of the 80 centers, 47 (58.7%) performed MRAK transplants less than expected, assuming a 22% MRAK transplant rate. Some centers who did no MRAK transplants had a 98% probability of performing one or more MRAK transplants. Median follow-up was 30 months. Kaplan-Meier (unadjusted) patient and graft survival at 1-, 2- and 3-years was 98.6% and 97.5%, 97.3% and 95.3%, and 96.7% and 93.2%, respectively, with conventional anatomy compared to 99.7% and 97.0%, 99.1% and 94.4%, and 98.2% and 92.6% with MRAK. (Figure 2) Risk of DCGF was approximately 2% higher with MRAK compared with conventional anatomy (1.3% vs 2.7%, 2.2% vs 4.7%, and 3.8% vs 5.6% at 1-,2-and 3-years, respectively; p=0.037). Cox’s random-effects model suggests the increased risk of DCGF may be driven by outcomes at one center.
*Conclusions: MRAK’s continue to be an important component of exchange programs, as they make up almost a quarter of transplants in the NKR. DCGF may be slightly higher in this population but this needs to be balanced against the risk of death on dialysis waiting for a kidney with conventional anatomy. Centers that do not perform transplants with MRAKs do not share fully the responsibility to disperse risk equally through-out the paired exchange program.
To cite this abstract in AMA style:
Roll GR, Irish W, Cooper M, Ronin M, Hil G, Waterman AD, Leeser DB. Social Loafing: Distribution of Kidneys with Multiple Renal Arteries in a National Paired Kidney Exchange Program [abstract]. Am J Transplant. 2019; 19 (suppl 3). https://atcmeetingabstracts.com/abstract/social-loafing-distribution-of-kidneys-with-multiple-renal-arteries-in-a-national-paired-kidney-exchange-program/. Accessed February 26, 2026.« Back to 2019 American Transplant Congress