Single-center Retrospective Analysis of Prophylaxis and Treatment of Pneumocystis Carinii Pneumonia in Patients with Poor Renal Function
Kidney-Pancreas Transplant Department., Tianjin First Central Hospital, Tianjin, China
Meeting: 2019 American Transplant Congress
Abstract number: D399
Keywords: Infection, Kidney transplantation, Lymphocytes, Renal dysfunction
Session Information
Session Name: Poster Session D: Late Breaking
Session Type: Poster Session
Date: Tuesday, June 4, 2019
Session Time: 6:00pm-7:00pm
 Presentation Time: 6:00pm-7:00pm
Presentation Time: 6:00pm-7:00pm
Location: Hall C & D
*Purpose: Pneumocystis carinii pneumonia (PcP) is a potentially life-threatening complication in renal transplant recipients. Although the use of trimethoprim-sulfamethoxazole (TMP-SMX) chemoprophylaxis after kidney transplantation is a widely accepted practice, more individualized approach toward the prescription of chemoprophylaxis has not been established due to the renal toxicity of TMP-SMX, especially for those recipients with renal dysfunction.
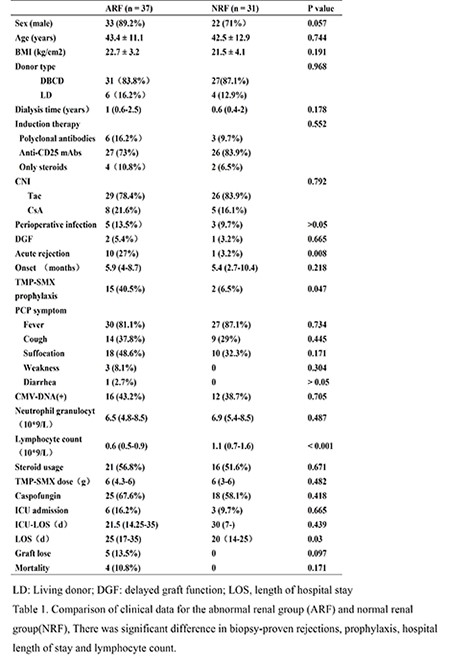
*Methods: We retrospectively analysed 68 cases of confirmed PcP, divided into an abnormal renal function(ARF) group(creatinine ≥ 132 umol/L; n = 37) and a normal renal function(NRF) group(creatinine < 132 umol/L; n = 31) . All organs were from deceased citizen donors or living donors and none were prisoners at the time of organ procurement. Comparing PCP characteristic and prognosis between two groups, the aim of this study is to propose the PCP individualized chemoprophylaxis and treatment strategies in recipients with renal dysfunction.
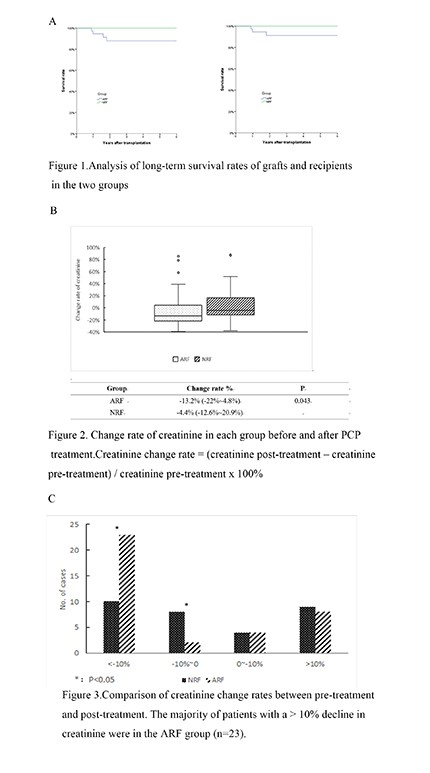
*Results: Compared with NRF group , patients in ARF group had more biopsy-proven rejections(10 [27%]Vs 1[3.2%],P=0.008), got more prophylaxis after transplantation(15[40.5%] Vs 2[6.5%],P=0.047),longer hospital length of stay(25[17-35]Vs 20[14-25],P=0.03), and lower lymphocyte count (0.6[05-0.9]Vs 1.1[0.7-1.6],p<0.01) (Table 1).There was no significant changes in creatinine levels between pre-treatment and post-treatment in 68 cases (135.5[110-170.5]Vs 125[104.8-164.5],P=0.132), but renal function had obviously improved in ARF group, which has a significant decrease rate in creatinine levels (-13.2%[-22%~4.8%]Vs-4.4%[-12.6%~ 20.9% ],P=0.043) (Figure 2). Moreover, the majority of patients with a > 10% decline in creatinine were in the ARF group (n = 23) (Figure 3).
*Conclusions: Renal function after renal transplantation should not be as a factor of deciding whether to administer a PCP chemoprophylaxis or treatment regimen. Patients with renal insufficiency after renal transplantation still need PCP chemoprophylaxis, and especially for those patients with acute rejection and persistent lymphopenia after transplantation.
To cite this abstract in AMA style:
Fu Y, Pan J, Shen Z. Single-center Retrospective Analysis of Prophylaxis and Treatment of Pneumocystis Carinii Pneumonia in Patients with Poor Renal Function [abstract]. Am J Transplant. 2019; 19 (suppl 3). https://atcmeetingabstracts.com/abstract/single-center-retrospective-analysis-of-prophylaxis-and-treatment-of-pneumocystis-carinii-pneumonia-in-patients-with-poor-renal-function/. Accessed February 25, 2026.« Back to 2019 American Transplant Congress