Sharp Anti-HLA Antibody Development Due to Concomitant Graft Nephrectomy and Immunosuppression Withdrawal After Early Graft Loss
1Nefrología, Hospital Universitario Marqués de Valdecilla, Santander, Spain, 2Inmunología, Hospital Universitario Marqués de Valdecilla, Santander, Spain
Meeting: 2021 American Transplant Congress
Abstract number: 944
Keywords: HLA antibodies, Immunosuppression, Nephrectomy, Waiting lists
Topic: Clinical Science » Kidney » Kidney Immunosuppression: Novel Regimens and Drug Minimization
Session Information
Session Name: Kidney Immunosuppression: Novel Regimens and Drug Minimization
Session Type: Poster Abstract
Session Date & Time: None. Available on demand.
Location: Virtual
*Purpose: The number of patients awaiting for retransplantation has been progressively increasing. The presence of anti-HLA antibodies can significantly lengthen the waiting time, limiting the access for a new transplant and increase the risk of graft rejection and failure. Risk factors for HLA sensitization are withdrawal of immunosuppression (IS) and graft nephrectomy (GN). GN is usually a non-elective procedure performed after early graft loss, mostly related to surgical complications or severe rejection. Currently there is no consensus on the discontinuation of immunosuppressive therapy after early graft nephrectomy.
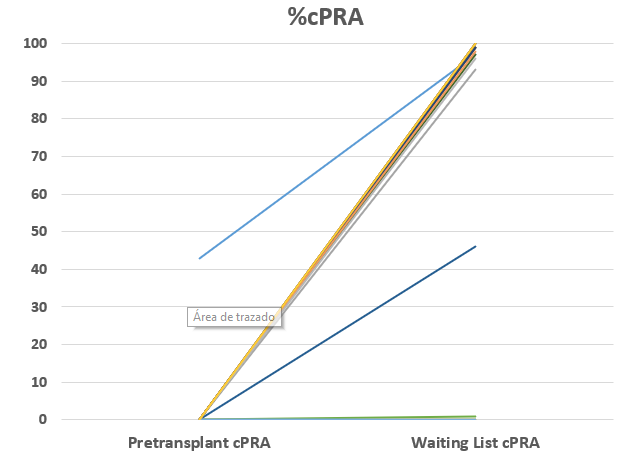
*Methods: Between 2014 and 2020 17 kidney grafts were removed at our center after early loss due to vascular thrombosis or bleeding. In 15 isolated kidney transplants (IKT), tacrolimus and mycophenolate were immediately withdrawn after GN and steroids were tapered in two weeks. In 2 simultaneous pancreas-kidney transplants (SPK) IS was maintained to preserve pancreas graft function. Anti-HLA antibodies were tested six months after graft loss using Single Antigen test. Calculated panel-reactive antibody (cPRA) was estimated using Virtual PRA Eurotransplant Calculator.
*Results: Pretransplant cPRA was 0% in all recipients but one (43%). Median cPRA 6-mo after GN was 98% (IQR 93%-99%), whereas both SPK transplants remained at 0%. Median difference between pretransplant and 6-mo post GN cPRA was 98% (IQR 54%-99%). Only 3 patients (20%) had a cPRA below 50% at the end of the study period (isolated kidney graft). Age, gender or induction therapy did not relate to development of anti-HLA antibodies (p = 0.712) whereas the presence of 2 DR-mismatches showed a higher trend to increased cPRA (98%±2% vs 57%±44%, p=0.072). Neither age nor gender related to a higher increase of cPRA.
*Conclusions: Early GN with rapid IS elimination is associated with almost universal severe HLA sensitization. This effect might be a direct consequence of IS elimination as it is not observed when IS is maintained. This fact should be considered when a new kidney transplant might be an option in the short/mid-term. Risk/benefit balance of IS maintenance on dialysis should be evaluated and it might be beneficial in selected cases.
To cite this abstract in AMA style:
Valero R, Aguilera A, Rodrigo E, Segundo DSan, Lopez-Hoyos M, Ruiz J. Sharp Anti-HLA Antibody Development Due to Concomitant Graft Nephrectomy and Immunosuppression Withdrawal After Early Graft Loss [abstract]. Am J Transplant. 2021; 21 (suppl 3). https://atcmeetingabstracts.com/abstract/sharp-anti-hla-antibody-development-due-to-concomitant-graft-nephrectomy-and-immunosuppression-withdrawal-after-early-graft-loss/. Accessed February 15, 2026.« Back to 2021 American Transplant Congress