Selectively Transplanting Moderately to Severely Macrosteatotic Grafts: Does Recipient Metabolic Environment Affect Outcomes?
P. J. Altshuler, A. Rios Diaz, O. Shaheen, A. P. Shah, W. R. Maley, A. Frank, C. Ramirez, J. Glorioso, H. Dang, A. S. Bodzin
Department of Surgery, Thomas Jefferson University, Philadelphia, PA
Meeting: 2020 American Transplant Congress
Abstract number: 44
Keywords: Donors, marginal, Dyslipidemia, Liver grafts, Metabolic disease
Session Information
Session Name: Liver: MELD, Allocation and Donor Issues (DCD/ECD) I
Session Type: Oral Abstract Session
Date: Saturday, May 30, 2020
Session Time: 3:15pm-4:45pm
 Presentation Time: 4:03pm-4:15pm
Presentation Time: 4:03pm-4:15pm
Location: Virtual
*Purpose: As incidence of Non-Alcoholic Steatohepatitis (NASH) cirrhosis rises, organ utilization remains stagnant. Recently, it has been shown that selective utilization of >30% macrosteatotic grafts can produce acceptable graft outcomes. We examine the effects of utilizing similarly metabolically impaired macrosteatotic donor grafts in NASH compared with non-NASH counterparts.
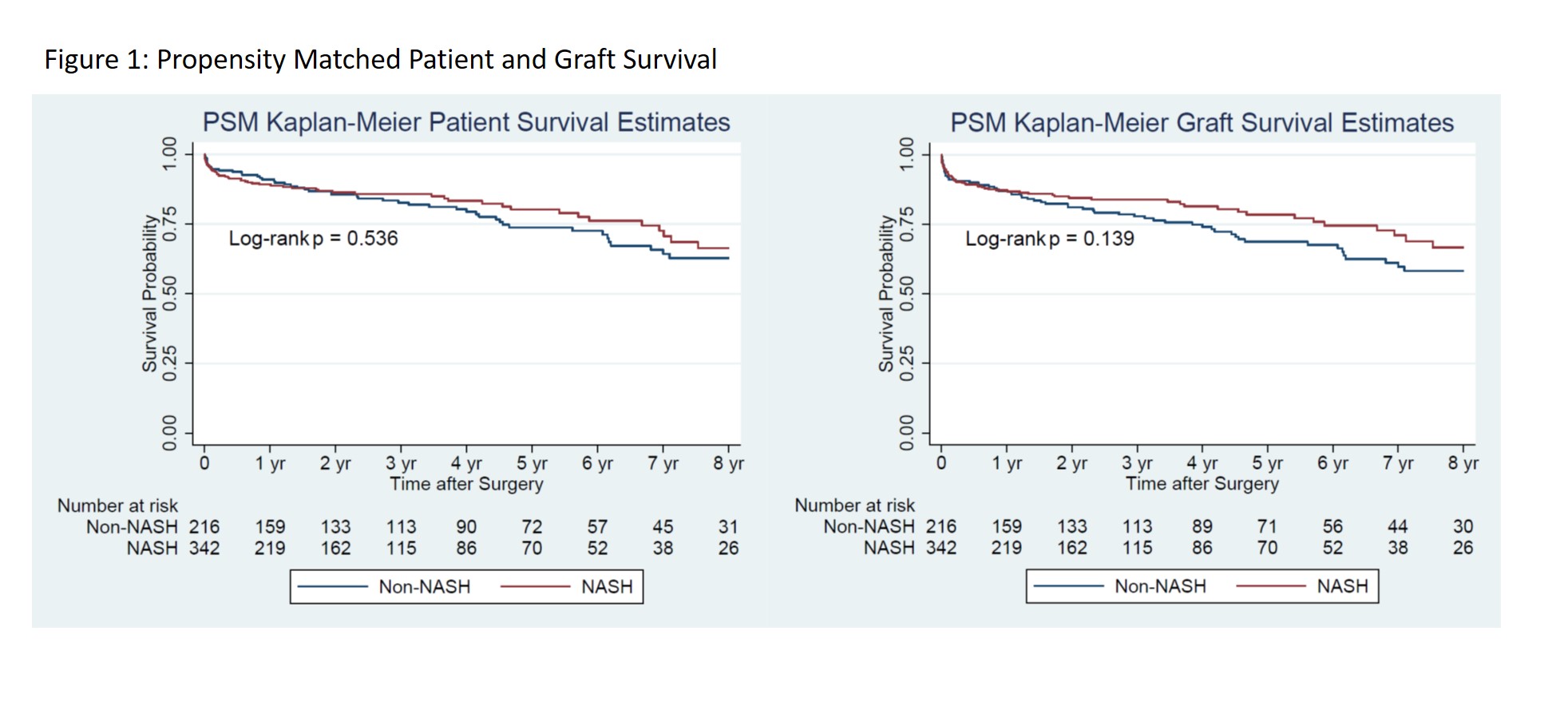
*Methods: Retrospective analysis of the Organ Procurement and Transplantation Network database from 2002 to 2019 identified 2,295 patients receiving >30% macrosteatotic grafts. Patients were stratified by diagnosis of NASH. Kaplan-Meier curves assessed survival with Cox proportional hazard and stratified log-rank tests assessing equality of survivor functions. Propensity score matching (PSM) addressed confounding variables.
*Results: NASH patients had higher unadjusted MELD scores (20 vs. 18, p<0.040), BMI (32 vs. 27, p<0.001), prevalence of diabetes (58.4% vs. 21.3%, p<0.001), portal vein thrombosis (PVT, 18.9 vs. 11.2%, p<0.001), and renal failure requiring dialysis (11.2% vs. 7.9%, p=0.046). PSM mitigated differences across MELD score, PVT, and renal failure, although trends in BMI and diabetes prevalence remained significant. PSM 1, 3 and 5-year patient survival were similar across NASH and non-NASH cohorts. Graft survival was similar at 1 and 3 years; however, NASH patients demonstrated significant improvement at 5 years. No difference was noted in mortality or graft failure on subgroup analysis including primary non-function (Figure 1).
*Conclusions: Despite differences in baseline characteristics and a more globally compromised profile, NASH patients tolerate macrosteatotic grafts as well as non-NASH counterparts. When matched, NASH demonstrated better 5-year survival with these grafts. Historically, transplants with >30% macrosteatotic grafts portend worse outcomes; short and long-term data here demonstrates these grafts have reasonable outcomes in populations with low incidences of primary non-function. These grafts can be safe to use in carefully selected donors in both NASH and non-NASH recipients.
| PSM Baseline Characteristics | NASH | Non-NASH | p-value | PSM Outcomes | NASH | Non-NASH | p-value |
| Age | 60 (55-65) | 60 (52-64) | 0.065 | Survival: 1 year | 308 (88.51%) | 198 (90.00%) | 0.679 |
| BMI | 32.1 (+/- 5.4) | 27.9 (+/- 5.5) | <0.001 | 3 years | 301 (86.49%) | 185 (84.09%) | 0.463 |
| Donor BMI | 33.6 (+/- 7.9) | 32.2 (+/- 7.8) | 0.041 | 5 years | 295 (84.77%) | 175 (79.55%) | 0.112 |
| MELD | 20 (15-25) | 20 (15-26) | 0.649 | Graft Survival: 1 year | 301 (86.49%) | 189 (85.91%) | 0.844 |
| Diabetes | 193 (58.31%) | 40 (18.86%) | <0.001 | 3 years | 294 (84.48%) | 174 (79.09%) | 0.113 |
| Renal Failure on Dialysis | 39 (11.21%) | 23 (10.45%) | 0.780 | 5 years | 288 (82.76%) | 163 (74.09%) | 0.013 |
| Portal Vein Thrombosis | 66 (19.02%) | 42 (19.18%) | 0.963 | Graft Primary Non-Function | 5 (1.44%) | 6 (2.73%) | 0.278 |
To cite this abstract in AMA style:
Altshuler PJ, Diaz ARios, Shaheen O, Shah AP, Maley WR, Frank A, Ramirez C, Glorioso J, Dang H, Bodzin AS. Selectively Transplanting Moderately to Severely Macrosteatotic Grafts: Does Recipient Metabolic Environment Affect Outcomes? [abstract]. Am J Transplant. 2020; 20 (suppl 3). https://atcmeetingabstracts.com/abstract/selectively-transplanting-moderately-to-severely-macrosteatotic-grafts-does-recipient-metabolic-environment-affect-outcomes/. Accessed February 25, 2026.« Back to 2020 American Transplant Congress