Role of Baseline PD-1 Checkpoint Inhibitor Pathway Expression in Bridge to Liver Transplant Hepatocellular Carcinoma
Ochsner Health, New Orleans, LA
Meeting: 2021 American Transplant Congress
Abstract number: 84
Keywords: Hepatocellular carcinoma, Immunosuppression, Risk factors, T cell activation
Topic: Clinical Science » Liver » Liver: Hepatocellular Carcinoma and Other Malignancies
Session Information
Session Name: Liver Transplant Oncology
Session Type: Rapid Fire Oral Abstract
Date: Saturday, June 5, 2021
Session Time: 6:00pm-7:00pm
 Presentation Time: 6:05pm-6:10pm
Presentation Time: 6:05pm-6:10pm
Location: Virtual
*Purpose: Response to first line liver-directed therapy (LDT) in hepatocellular carcinoma (HCC) has important implications in both bridge to transplant (BTT) success as well as post-transplant recurrence-free survival. An effective anti-tumoral T cell response following LDT is a critical barrier against tumor progression. In this study, we investigated baseline T cell count and the PD-1 checkpoint inhibitory pathway as indicators of T cell exhaustion and the role in LDT response and BTT outcome.
*Methods: Treatment-naïve HCC patients receiving LDT were prospectively enrolled. Preprocedural peripheral blood was collected and T cells characterized for lineage and phenotype by flow cytometry. LDT response was assessed by mRECIST.
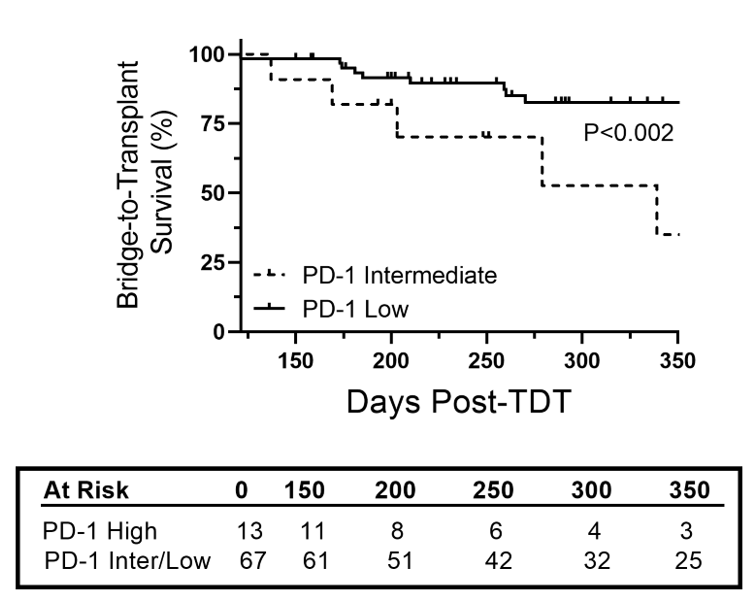
*Results: Univariate analysis of the cohort (n=86) confirmed incomplete response to first line LDT (P=0.003, OR 7.6) was closely associated with BTT survival and waitlist tumor progression (P<0.001). We then performed univariate analysis to identify T cell-linked factors associated with an incomplete response to LDT. Pre-treatment absolute lymphocyte count (ALC) (P=0.009, OR 0.44) as well as CD4:CD8 lineage specific PD-1 expression (P=0.043, OR 3.0 and P=0.010, OR 3.3 respectively) were associated with risk of incomplete response. LDT-induced decrease in PD-1 expression in CD8 T cells in patients with elevated PD-1 at baseline (P<0.001) while a LDT-induced increase in PD-1 expression was observed in CD4 T cells in patients with low baseline PD-1 expression (P=0.018). Further, elevated PD-1 expression was associated with increased risk of BTT tumor progression (P=0.002, HR = 4.6, 95%CI 1.7-11.7). In patient’s successfully bridged to liver transplantation, an elevated PD-1 expression profile at baseline or follow-up was associated with advanced tumor staging (P<0.001), with 75% of PD-1 high patients having T3-T4 TNM staging compared to 0% with intermediate/low PD-1 expression.
*Conclusions: Low lymphocyte count and activation of the PD-1 checkpoint inhibitor pathway is associated with risk of incomplete response to LDT and waitlist tumor progression. Patients with impaired T cell homeostasis may benefit from adjuvant immunotherapy to improve response to LRT and improve bridge to transplant outcomes.
To cite this abstract in AMA style:
Nunez K, Sandow T, Hibino M, Cohen A, Thevenot P. Role of Baseline PD-1 Checkpoint Inhibitor Pathway Expression in Bridge to Liver Transplant Hepatocellular Carcinoma [abstract]. Am J Transplant. 2021; 21 (suppl 3). https://atcmeetingabstracts.com/abstract/role-of-baseline-pd-1-checkpoint-inhibitor-pathway-expression-in-bridge-to-liver-transplant-hepatocellular-carcinoma/. Accessed March 5, 2026.« Back to 2021 American Transplant Congress