Risk Stratification of Kidney Transplant Patients According to the Different Level of HLA-DQ Disparities
1Microbiology, Immunology and Transplantation, KU Leuven, Leuven, Belgium, 2Northwestern University, Chicago, IL
Meeting: 2021 American Transplant Congress
Abstract number: 216
Keywords: Graft survival, HLA matching, Kidney transplantation, MHC class II
Topic: Basic Science » Histocompatibility and Immunogenetics
Session Information
Session Name: B cell/Antibody and Histocompatibility
Session Type: Rapid Fire Oral Abstract
Date: Monday, June 7, 2021
Session Time: 4:30pm-5:30pm
 Presentation Time: 5:05pm-5:10pm
Presentation Time: 5:05pm-5:10pm
Location: Virtual
*Purpose: It is becoming clear that de novo donor-specific antibodies (dnDSA) against HLA-DQ are the most prevalent and the leading cause of chronic antibody-mediated rejection and poor allograft outcome after kidney transplantation. A well-known problem with the most HLA matching approaches is that they don’t include systematic genotyping of HLA-DQ locus. Herein we evaluate the role of HLA-DQ matching at antigen, allele and haplotype levels to minimize the generation of HLA-DQ-dnDSA and improve graft outcome in kidney transplantation.
*Methods: All adult patients who underwent kidney transplantation between 2004 and 2013 at a single center, with available DNA samples were included in this study (N=926). Each transplant pair was retrospectively genotyped at the 2nd field HLA level for HLA-DQA1 and HLA-DQB1.
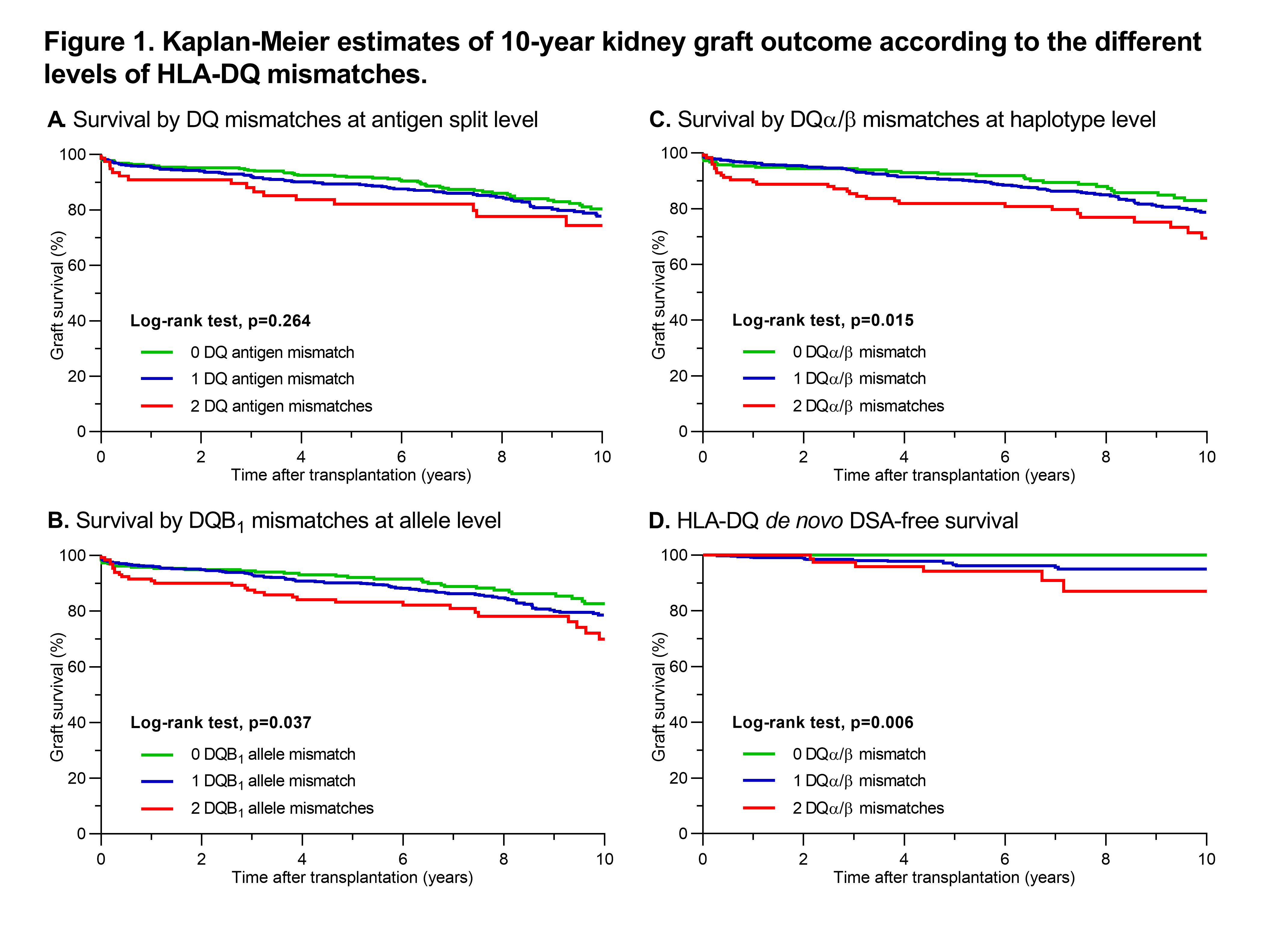
*Results: The mean follow-up time of this kidney transplant cohort was 7.62 ± 3.78 years. 152 patients (16.4%) experienced graft failure during this period. HLA-DQ dnDSA occurred in 23 of 889 patients with antibody follow-up data within the first ten years. Figure 1 depicts the 10-year graft survival Kaplan-Meier curves according to the different levels of HLA-DQ MM. The 10-year survival rates were not statistically different between the groups with 0, 1 and 2 DQ antigen MM (80.4%, 77.7% and 74.3% respectively, p=0.27). In contrast, the different degrees of allele mismatches for the DQB1 locus provided better risk stratification of the patients (82.8% with 0 DQB1 MM, 78.6% with 1 DQB1 MM and 70.0% with 2 DQB1 MM, p=0.04). Next, we calculated the mismatches in the DQα/β pairs by considering DQA1 at the 1st and DQB1 at the 2nd field HLA genotyping level. The Kaplan-Meier curves showed that primarily the degree of mismatches for DQα/β haplotypes associated with the risk of graft failure after kidney transplantation (83.0% with 0 DQα/β MM, 78.7% with 1 DQα/β MM and 69.4% with 2 DQα/β MM, p=0.02). Finally, the patients with both matched DQα/β haplotypes had 100% DQ dnDSA-free survival compared to the decreased DQ dnDSA-free survival in patients with one (95.1%) or both (87.1%) mismatched DQα/β haplotypes (p=0.006).
*Conclusions: By comparing the HLA-DQ mismatches at antigen, allele and haplotype levels, we found that DQα/β haplotype mismatch analysis provides the best risk stratification of the kidney transplant patients. These findings indicate that adding DQα/β haplotype matching to the current antigen HLA-A, -B, or -DR matching algorithm will decrease de novo formation of HLA-DQ antibodies and improve graft survival after kidney transplantation.
To cite this abstract in AMA style:
Senev A, Tambur AR, Naesens M. Risk Stratification of Kidney Transplant Patients According to the Different Level of HLA-DQ Disparities [abstract]. Am J Transplant. 2021; 21 (suppl 3). https://atcmeetingabstracts.com/abstract/risk-stratification-of-kidney-transplant-patients-according-to-the-different-level-of-hla-dq-disparities/. Accessed February 28, 2026.« Back to 2021 American Transplant Congress