Risk Factors for Extubation Failure Post- Lung Transplantation
1Allergy, Pulmonary and Critical Care Medicine, Vanderbilt University Medical Center, Nashville, TN, 2Thoracic Surgery, Vanderbilt University Medical Center, Nashville, TN
Meeting: 2022 American Transplant Congress
Abstract number: 1466
Keywords: Lung transplantation, Mechnical assistance, Risk factors, Surgical complications
Topic: Clinical Science » Lung » 64 - Lung: All Topics
Session Information
Session Time: 7:00pm-8:00pm
 Presentation Time: 7:00pm-8:00pm
Presentation Time: 7:00pm-8:00pm
Location: Hynes Halls C & D
*Purpose: Extubation delays following lung transplantation can result in delirium, deconditioning, infections, and increased hospital length of stay. Risk stratifying patients for extubation failure may allow for improved candidate selection and optimal pre-and post-transplant management, including early tracheostomy. Identifying limitations to timely extubation post-transplant remains understudied.
*Methods: We performed a single-center retrospective analysis of lung allograft recipients (LTRs) age >18 years that were transplanted between 1/2018- 10/2021 to identify pre- and peri-operative risk factors for extubation failure. Extubation failure was defined as inability to liberate from invasive mechanical ventilation (IMV) within 72 hours post-transplant, or re-intubation within 72 hours of extubation. Statistical analysis was performed using STATA v. 15.1. Differences were assessed using Fisher’s exact test for binary data, Pearson’s chi-square test for categorical variables and Mann-Whitney U-test for continuous data. Multivariate logistic regression analyses were performed using clinically meaningful covariates that were significant on univariate assessment at p<0.01.
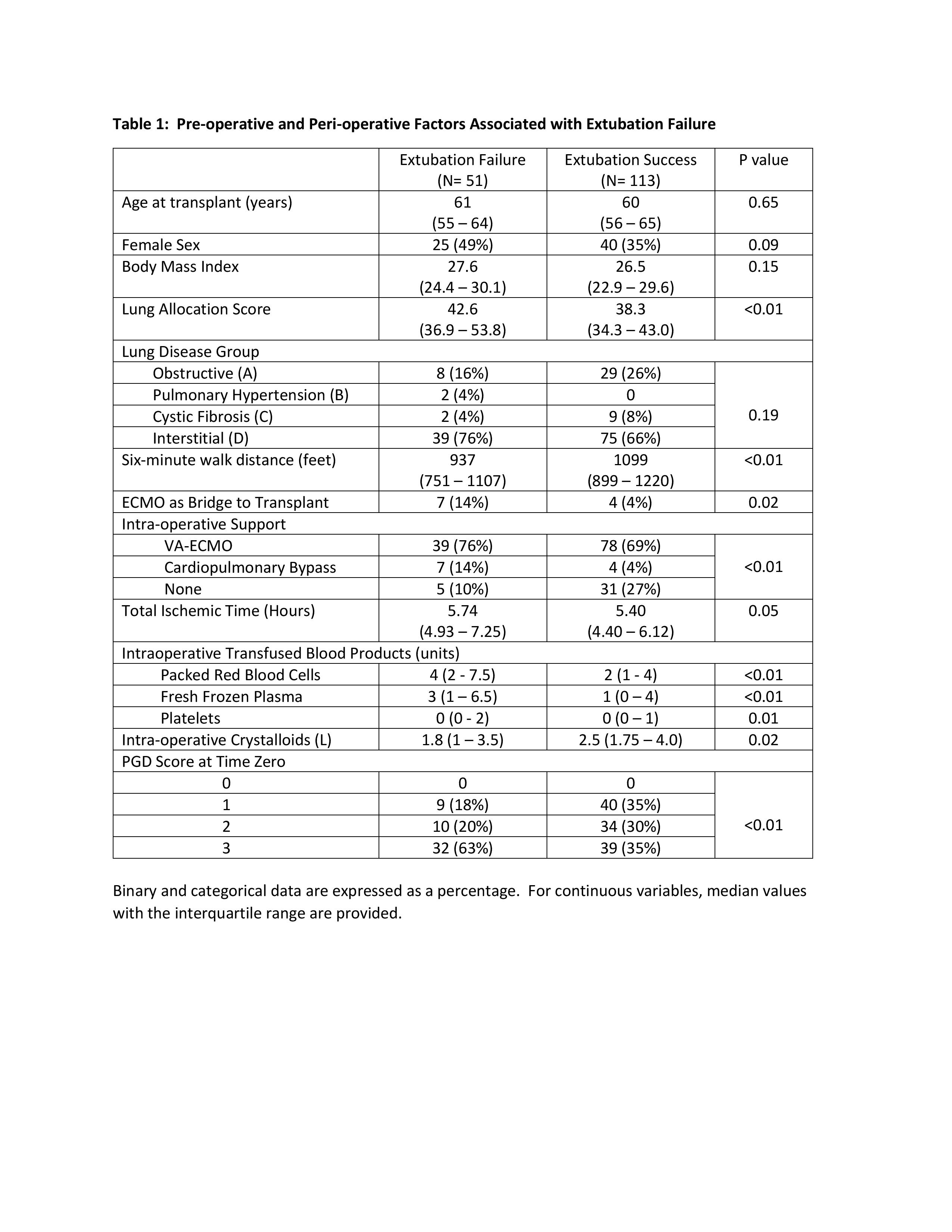
*Results: 164 LTRs were included; 51 met criteria for extubation failure while 113 patients were successfully liberated from IMV. There was a significant difference in lung allocation score, six-minute walk distance (6MWD), need for pre- and peri-operative mechanical support, intra-operative blood transfusion and post-operative primary graft dysfunction (PGD@T0) between cohorts (p <0.05, see Table 1). There were no differences in age, gender, body mass index, race, lung disease, forced vital capacity, pulmonary artery pressure, transplant type, ischemic time, and donor microorganism colonization between groups. PGD (T0) and red blood cell (PRBC) transfusions were associated with extubation failure after adjusting for peri-operative mechanical support need and 6MWD (OR: 1.80 95% CI: 1.14 to 2.84; p=0.01 and OR: 1.1 95% CI: 1.02 to 1.21; p=0.01 respectively).
*Conclusions: Greater intra-operative PRBC transfusion and higher PGD at T0 are associated with post- lung transplant extubation failure.
To cite this abstract in AMA style:
Trindade AJ, Gannon WD, Dragnich AG, Dahlberg G, Demarest CT, Lambright ES, McPherson KA, Norfolk SG, Shaver CM, Robbins IM, Bacchetta M. Risk Factors for Extubation Failure Post- Lung Transplantation [abstract]. Am J Transplant. 2022; 22 (suppl 3). https://atcmeetingabstracts.com/abstract/risk-factors-for-extubation-failure-post-lung-transplantation/. Accessed February 26, 2026.« Back to 2022 American Transplant Congress