Retransplantation after Living Donor Liver Transplantation: Analysis of Data from the A2ALL Study
Surgery, University of California, San Francisco, San Francisco, CA.
Meeting: 2018 American Transplant Congress
Abstract number: 243
Keywords: Liver, Retransplantation
Session Information
Session Name: Concurrent Session: Liver Retransplantation and Other Complications
Session Type: Concurrent Session
Date: Monday, June 4, 2018
Session Time: 2:30pm-4:00pm
 Presentation Time: 3:18pm-3:30pm
Presentation Time: 3:18pm-3:30pm
Location: Room 6A
Living donor liver transplantation (LDLT) is associated with a higher incidence of post-transplant vascular and biliary complications. Outcomes for retransplantation (reLT) after LDLT are not well understood; this study reviewed the need for reLT following LDLT using data from the Adult to Adult Living Donor Liver Transplantation Study (A2ALL).
Recipients in the A2ALL cohort who underwent LDLT between April 1998 and January 2014 were included. We compared LDLT followed by reLT to LDLT alone. Descriptive analysis was performed using Wilcoxon rank sum and chi-squared tests; patient survival was estimated using Kaplan-Meier methods.
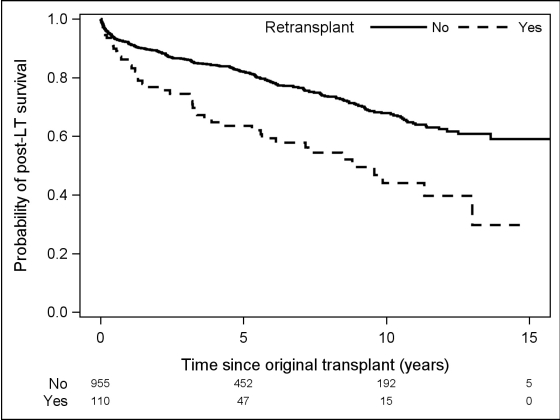
1065 recipients were included. 110 recipients (10.3%) required reLT following initial LDLT. reLT patients were predominantly male (65.5%), Caucasian (94.5%), median (IQR) age of 49.2 years (40.9-57.3), median BMI 25 (23-28), and median MELD 16 (12-20). The majority were right lobe recipients (93.6%) and related to their donor (59.1%). Compared with patients who underwent LDLT alone, reLT patients were slightly younger (49.2 vs. 52.8 years, p=0.001) and had a higher total bilirubin at the time of LDLT (3.1 vs. 2.6, p=0.02). The most common cause of graft failure was vascular thrombosis (47.8%) followed by primary graft failure (19.4%), other (13.4%), and recurrent hepatitis (10.4%). ReLT patients had a longer length of stay in the hospital (18 vs. 10, p<0.001) and ICU (3 vs. 1 days, p<0.001) after initial LDLT, and a greater number of complications (5 vs. 3, p<0.001). Patient survival after initial LDLT was significantly lower for reLT vs LDLT alone (p<0.001). Survival (95% CI) for reLT and LDLT patients, respectively, was 86.2% (78-92) vs. 91.6% (90-93) at 1-year, 63.5% (53-73) vs. 81.9% (79-85) at 5-years, and 44.1% (31-56) vs. 67.9% (64-72) at 10-years (Figure 1).
Vascular thrombosis and primary graft failure are the most common indications for reLT following LDLT. ReLT after LDLT is associated with significantly worse patient survival at 5 and 10 years post-transplant. ReLT poses a complex ethical and emotional dilemma for the transplant team.
CITATION INFORMATION: Braun H., Grab J., Dodge J., Syed S., Roll G., Freise C., Roberts J., Ascher N. Retransplantation after Living Donor Liver Transplantation: Analysis of Data from the A2ALL Study Am J Transplant. 2017;17 (suppl 3).
To cite this abstract in AMA style:
Braun H, Grab J, Dodge J, Syed S, Roll G, Freise C, Roberts J, Ascher N. Retransplantation after Living Donor Liver Transplantation: Analysis of Data from the A2ALL Study [abstract]. https://atcmeetingabstracts.com/abstract/retransplantation-after-living-donor-liver-transplantation-analysis-of-data-from-the-a2all-study/. Accessed March 6, 2026.« Back to 2018 American Transplant Congress