Restrictive Medicaid Policies Reduce Access to Liver Transplant for Alcohol-Associated Liver Disease
UCSF, SF, CA
Meeting: 2019 American Transplant Congress
Abstract number: D396
Session Information
Session Name: Poster Session D: Late Breaking
Session Type: Poster Session
Date: Tuesday, June 4, 2019
Session Time: 6:00pm-7:00pm
 Presentation Time: 6:00pm-7:00pm
Presentation Time: 6:00pm-7:00pm
Location: Hall C & D
*Purpose: Medicaid policies requiring specific documentation of abstinence (e.g. 6 months) and/or rehabilitation for financial coverage of liver transplant (LT) for alcohol-associated liver disease (ALD) vary by state. How these policies affect LT rates for ALD, particularly with the emergence of early LT practices since 2011, are not well described.
*Methods: Medicaid policies for states performing adult LTs in 2017 were categorized as “restricted” vs. “unrestricted”, confirmed directly by state Medicaid offices or transplant physicians. “Restricted” was defined as requiring documentation of a specific period of abstinence and/or rehabilitation. Medicaid policies that deferred to center eligibility policies were categorized as “unrestricted”. All UNOS adult LT recipients from 2002-2017 with ALD as primary listing diagnosis were included; HCC, MELD exceptions, unknown insurance status were excluded. Alcoholic hepatitis (AH) centers included all centers that performed at least 1 LT with a primary listing diagnosis of AH since 2011. Logistic regression was used to assess the effect of restrictive policies after 2011 on payment by Medicaid for LTs among patients with ALD.
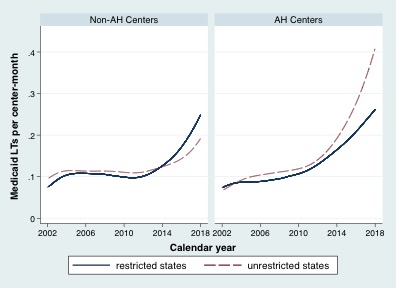
*Results: A total of 10,836 LT recipients for ALD from 2002-2017, with 6,972 from 23 states in restricted policy group and 3,864 from 15 states in unrestricted group. Adjusted rates per center-month of LTs for ALD paid by Medicaid are shown in Figure 1. In models adjusting for individual-level characteristics affecting likelihood of LT, region wait-time, differences by period in unrestricted states, and differences between restricted and unrestricted states in 2002-11, restricted policy was associated with lower odds of LT for ALD in Medicaid 2012-17 (OR 0.74, 95% CI 0.57-0.96, p=0.02). In stratified analysis, this association was nominally stronger at AH (OR 0.67, 95% CI 0.46-0.98, p=0.04) than at non-AH centers (OR 0.82, 95% CI 0.57-1.20, p=0.31; interaction p=0.21).
*Conclusions: Restrictive Medicaid policies are present in the majority of states with active LT centers, and are associated with reductions in payment by Medicaid for LT in ALD since 2011, compared to states without restrictive Medicaid policies. This disparity may be larger at centers performing LT for AH. Re-evaluation of Medicaid policy may help eliminate this disparity.
To cite this abstract in AMA style:
Lee BP, Eric V, Mark P, Dodge J, Terrault N. Restrictive Medicaid Policies Reduce Access to Liver Transplant for Alcohol-Associated Liver Disease [abstract]. Am J Transplant. 2019; 19 (suppl 3). https://atcmeetingabstracts.com/abstract/restrictive-medicaid-policies-reduce-access-to-liver-transplant-for-alcohol-associated-liver-disease/. Accessed March 3, 2026.« Back to 2019 American Transplant Congress