Recipient and Center Factors Associated with Immunosuppression Practice Beyond the First Year After Liver Transplantation
1University of Pennsylvania, Philadelphia, PA, 2University of Miami, Miami, FL
Meeting: 2022 American Transplant Congress
Abstract number: 1088
Keywords: Immunosuppression, Liver
Topic: Clinical Science » Liver » 54 - Liver: Immunosuppression and Rejection
Session Information
Session Name: Liver: Immunosuppression and Rejection
Session Type: Poster Abstract
Date: Sunday, June 5, 2022
Session Time: 7:00pm-8:00pm
 Presentation Time: 7:00pm-8:00pm
Presentation Time: 7:00pm-8:00pm
Location: Hynes Halls C & D
*Purpose: To investigate patient and center factors associated with differences in immunosuppression management in the first 5 years after LT.
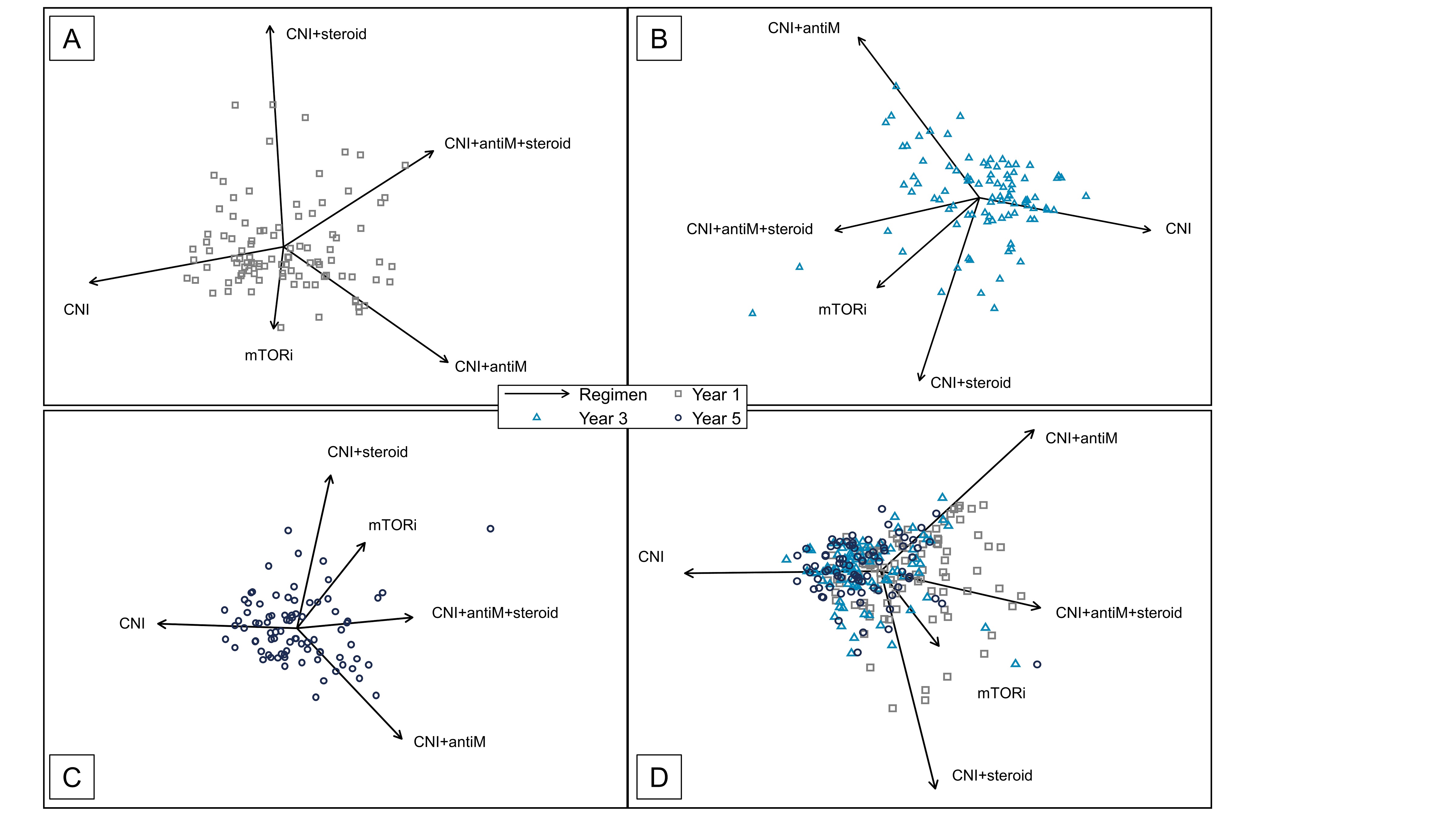
*Methods: A retrospective cohort of 11,326 adult first LT alone recipients between 2007-2016 was identified by linking United Network for Organ Sharing (UNOS) transplant data to Medicare administrative claims. Immunosuppression regimen was obtained from Medicare drug billing claims. Predictors of calcineurin inhibitor (CNI) monotherapy at 1-, 3- and 5-years post-LT were investigated using multivariable mixed-effects logistic regression. Center heterogeneity in management was evaluated visually using biplots.
*Results: The UNOS-Medicare cohort accounted for 23.1% of all adult first LT alone recipients in the US during the study period and was largely representative. CNI monotherapy was achieved in 56.4% at 1-year and 71.6% at 5-years post-LT, while center-specific CNI monotherapy rates ranged from 22.5-84.3% and 20.5%-95.2%, respectively. Increasing center CNI dominance and decreasing center heterogeneity from year 1 to year 5 post-LT is shown in the Figure. The majority of patients achieving CNI monotherapy at 1-year remained on this regimen at 3- and 5-years (88.8% and 87.4%). Black race was independently associated with a lower likelihood of CNI monotherapy at 1-, 3- and 5-years post-LT (adjusted OR 0.81 [p=0.036], OR 0.74 [p=0.018], OR 0.73 [p=0.046] respectively vs White), as well as an increased odds of therapy escalation between years 1-3 (adjusted OR 1.42; p=0.020). Early acute rejection decreased the odds of CNI monotherapy at 1-year post-LT (0.76; p<0.001) but not at 3- and 5-years post-LT (p=0.140 and p=0.578).
*Conclusions: In this first large-scale and contemporary analysis of LT immunosuppression practices in the first 5 years post-transplant, a considerable subset of recipients remained on long-term multi-drug therapy. Center heterogeneity in practice was observed. Further research is needed to ascertain the impact of these differences on post-LT outcomes.
To cite this abstract in AMA style:
Bittermann T, Goldberg D. Recipient and Center Factors Associated with Immunosuppression Practice Beyond the First Year After Liver Transplantation [abstract]. Am J Transplant. 2022; 22 (suppl 3). https://atcmeetingabstracts.com/abstract/recipient-and-center-factors-associated-with-immunosuppression-practice-beyond-the-first-year-after-liver-transplantation/. Accessed February 19, 2026.« Back to 2022 American Transplant Congress