Reassessing Tubulitis and Interstitial Infiltrate: Creating a New Probabilistic Definition of TCMR
Alberta Transplant Applied Genomics Centre, Edmonton, Canada.
Meeting: 2015 American Transplant Congress
Abstract number: D166
Keywords: Biopsy, Kidney transplantation, Rejection
Session Information
Session Name: Poster Session D: Kidney: Acute Rejection
Session Type: Poster Session
Date: Tuesday, May 5, 2015
Session Time: 5:30pm-6:30pm
 Presentation Time: 5:30pm-6:30pm
Presentation Time: 5:30pm-6:30pm
Location: Exhibit Hall E
Conventional diagnosis of T cell-mediated rejection (TCMR) in kidney transplant biopsies relies on interstitial inflammation (i-lesions), tubulitis (t-lesions), vasculitis (v-lesions) and experience-derived interpretation rules. The accuracy of these criteria for true TCMR is unknown because there has been no histology-independent test. The availability of a validated molecular test for TCMR presents an opportunity to compare various histologic criteria for their relative ability to predict molecular TCMR. In 703 prospective indication biopsies three days to 35 years post transplant, random forests and decision tree analysis indicated that i- and t-lesions were the best predictors of TCMR scores; v-lesions were much less important (Figure 1A). In tree analysis the relationship of i-/t-scores to TCMR was probabilistic rather than based on current cutoffs such as i>1/t>1 (Figure 1B). The recorded i- and t-lesions predicted molecular TCMR better than the recorded diagnosis, which sometimes missed TCMR when other diseases were present. The probability of positive TCMR scores in conventional TCMR depended on the actual lesions: 95% with i>1/t>1v>0; 57% with i>1/t>1 but v=0; 22% for isolated v; 25% for borderline. Biopsies without TCMR lesions (i-score 0, t-score 0, v-score 0) were 98% TCMR score negative. The probability that “Borderline” represented TCMR was time dependent: 27% <1 year; 19% 1-5 years; and 2% after 5 years (Table 1). Thus i- and t-lesions are the hallmark of TCMR, but a probabilistic approach based on actual recorded lesions and time will better reflect true TCMR, with molecular testing required in uncertain cases. 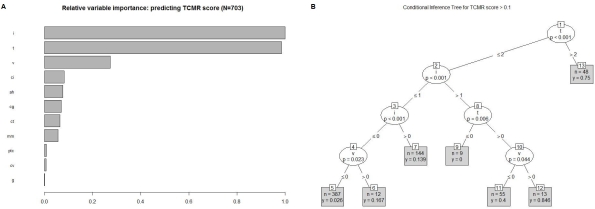
| # Conventional lesion-based diagnoses (#TCMR score +ve) | <1 yr | 1-5yrs | >5 yr | Total |
| All TCMR/Mixed | 68 (43) | 22 (16) | 19 (3) | 109 (62) |
| i>1/t>1/v>0 | 16 (16) | 5 (4) | 0 (0) | 21 (20) |
| i>1/t>1/v=0 (or v missing) | 40 (25) | 12 (9) | 8 (2) | 60 (36) |
| isolated v | 12 (2) | 5 (3) | 11 (1) | 28 (6) |
| Borderline | 67 (18) | 58 (11) | 47 (1) | 172 (30) |
| Inflamed (i) with no tubulitis | 17 (3) | 15 (1) | 25 (1) | 57 (5) |
| i0t0v0* | 146 (5) | 92 (1) | 124 (1) | 346 (7) |
| TOTAL | 298 (69) | 190 (29) | 215 (6) | 703 (104) |
To cite this abstract in AMA style:
Halloran P, Salazar I, Lopez M, Chang J. Reassessing Tubulitis and Interstitial Infiltrate: Creating a New Probabilistic Definition of TCMR [abstract]. Am J Transplant. 2015; 15 (suppl 3). https://atcmeetingabstracts.com/abstract/reassessing-tubulitis-and-interstitial-infiltrate-creating-a-new-probabilistic-definition-of-tcmr/. Accessed February 20, 2026.« Back to 2015 American Transplant Congress
