Re-Transplantation Outcomes in the United States Before and after DAA-Introduction
Surgery, Henry Ford Hospital, Detroit, MI
Meeting: 2020 American Transplant Congress
Abstract number: C-149
Keywords: Hepatitis C, Liver grafts, Liver transplantation, Retransplantation
Session Information
Session Name: Poster Session C: Liver Retransplantation and Other Complications
Session Type: Poster Session
Date: Saturday, May 30, 2020
Session Time: 3:15pm-4:00pm
 Presentation Time: 3:30pm-4:00pm
Presentation Time: 3:30pm-4:00pm
Location: Virtual
*Purpose: The success of direct-acting antiviral (DAA) therapy has led to the widespread treatment of HCV and near-universal cure for chronically infected patients and improved both graft and patient survival after liver transplantation (LT). Historically, the incidence of liver re-transplantation (re-LT) approaches 22%. We sought to investigate the trends and outcomes of re-transplantation in HCV patients in the United States before and after the introduction of DAA.
*Methods: Adult patients who underwent re-LT were identified in the OPTN/UNOS database. Multi-organ transplant patients, pediatric patients, and patients with more than two total transplants were excluded. Two eras were defined according to the introduction of DAA therapy, pre-DAA (2010 through 2013), and post-DAA (2014 through 2017). Survival was evaluated using the Kaplan-Meier method. Multivariable Cox regression was performed to identify potential predictors of post-re-LT mortality.
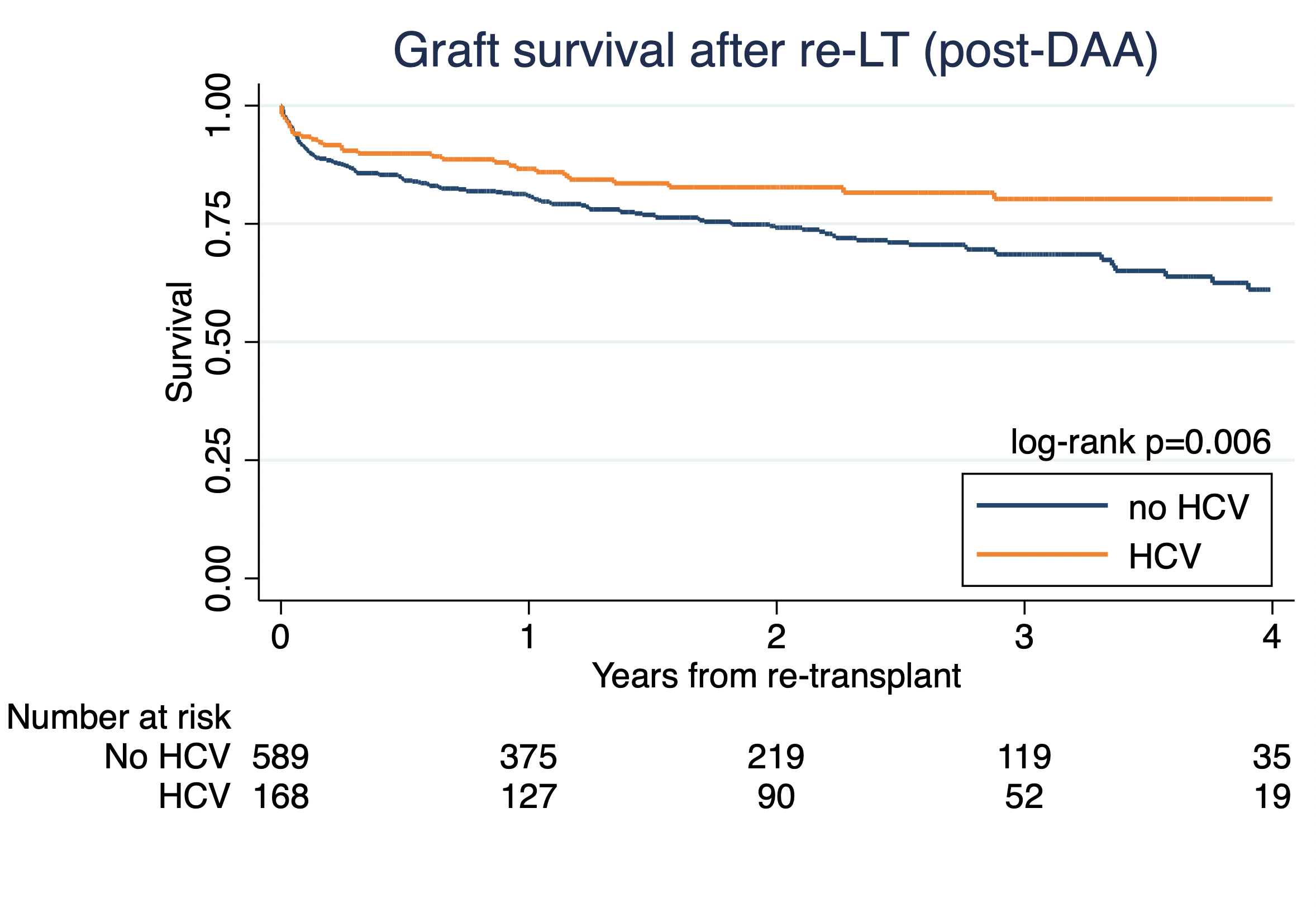
*Results: The query identified 1,600 patients who underwent re-LT (pre-DAA n=826 vs. post-DAA n=774). There were more HCV patients who underwent re-LT in the pre-DAA era (pre-DAA 253 (30.6%) vs. post-DAA 171 (22.1%); p<0.001). HCV patients who underwent re-LT in both pre- and post-DAA eras were more likely to experience hepatitis recurrence as a contributing cause of graft failure (pre-DAA HCV 94 (59.1%) vs. no HCV 48 (9.1%); p<0.001 and post-DAA HCV 32 (18.7%) vs. no HCV 27 (4.5%); p<0.001. Other causes of primary graft failure requiring re-LT were similar between groups. In the Pre-DAA era, HCV patients had similar graft survival as non-HCV patients (Fig.1). In the post-DAA era, HCV patients had improved post-graft survival compared to non-HCV patients (Fig.2). Multivariable analysis identified HCV to have a similar risk for graft failure (HR 0.96, 95% CI 0.70-1.32; p=0.80) as non-HCV patients in the pre-DAA era. In the post-DAA era, HCV represented an independent protective factor for graft survival (HR 0.45, 95% CI 0.27-0.74; p=0.002).
*Conclusions: After the introduction of DAA, HCV patients have improved graft survival compared to other etiologies following re-transplantation.
To cite this abstract in AMA style:
Ivanics T, Rizzari M, Al-Kurd A, Kitajima T, Elsabbagh A, Collins K, Yoshida A, Abouljoud M, Nagai S. Re-Transplantation Outcomes in the United States Before and after DAA-Introduction [abstract]. Am J Transplant. 2020; 20 (suppl 3). https://atcmeetingabstracts.com/abstract/re-transplantation-outcomes-in-the-united-states-before-and-after-daa-introduction/. Accessed February 21, 2026.« Back to 2020 American Transplant Congress