Racial/Ethnic Disparities in Rates of Living Donor Liver Transplant Are Partly Explained by Socioeconomic Deprivation in Adults
Johns Hopkins University School of Medicine, Baltimore, MD
Meeting: 2022 American Transplant Congress
Abstract number: 1200
Keywords: Liver transplantation, Multivariate analysis
Topic: Clinical Science » Organ Inclusive » 70 - Non-Organ Specific: Disparities to Outcome and Access to Healthcare
Session Information
Session Name: Non-Organ Specific: Disparities to Outcome and Access to Healthcare
Session Type: Poster Abstract
Date: Sunday, June 5, 2022
Session Time: 7:00pm-8:00pm
 Presentation Time: 7:00pm-8:00pm
Presentation Time: 7:00pm-8:00pm
Location: Hynes Halls C & D
*Purpose: Living donor liver transplant (LDLT) is an important strategy for addressing the deceased donor liver shortage and is associated with improved survival but represents <5% of LT in the United States. Despite these benefits, rates of LDLT remain low especially among non-White LT candidates and candidates with public insurance. In pediatric LT, racial/ethnic disparities in waitlist outcomes are partly explained by socioeconomic deprivation. We evaluated whether socioeconomic deprivation mediated associations between race/ethnicity and LDLT rates in adults.
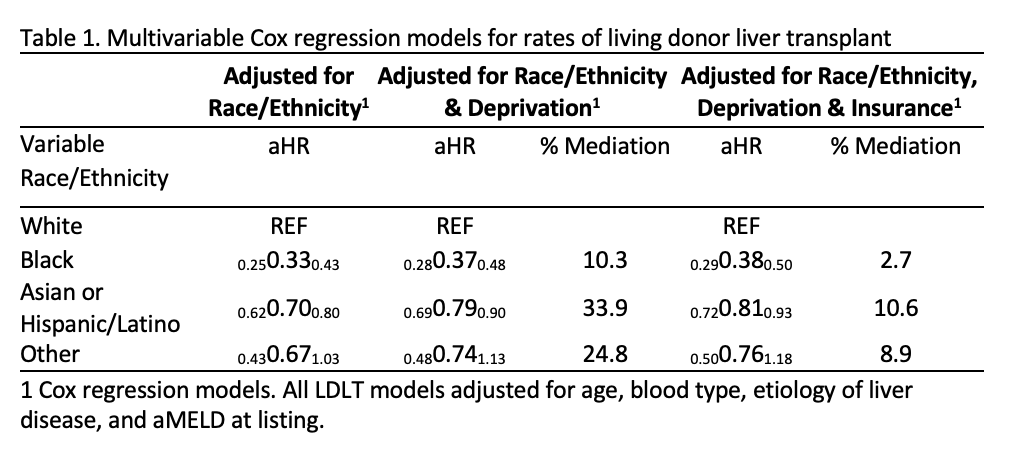
*Methods: SRTR was queried for adults (>18 years) who were listed for LT 2014-2021. Patients who were listed for multi-organ transplant were excluded. SRTR data was linked at the ZIP code level to a neighborhood socioeconomic deprivation index. We used Cox regression and Baron/Kenny to check potential mediation of race/ethnicity and LDLT associations by socioeconomic deprivation and insurance type, adjusting for age, blood type, etiology of liver disease, and aMELD at listing.
*Results: 64,214 LT candidates with ZIP code data available in SRTR were included of which 71.6% were White, 7.1% Black, 19.7% Asian or Hispanic/Latino, and 1.6% other. Compared to White candidates, Black, Asian and Hispanic/Latino, and other candidates had decreased incidence of LDLT (aHR 0.33, 95% CI 0.25-0.43; aHR 0.70, 95% CI 0.62- 0.80 and aHR 0.65, 95% CI 0.43- 1.03, respectively). After adjusting for deprivation index and insurance type, Black, Asian and Hispanic/Latino, and other candidates continued to have decreased, but slightly attenuated incidence of LDLT (aHR 0.38, 95% CI 0.29- 0.50; aHR 0.81, 95% CI 0.72- 0.93 and aHR 0.75, 95% CI 0.50- 1.18, respectively).
*Conclusions: The association between race/ethnicity and rates of LDLT was attenuated after adjusting for neighborhood socioeconomic deprivation, suggesting partial mediation. A complex approach to understanding how social factors contribute to disparity in LDLT is necessary to inform initiatives aimed at increasing LDLT in underrepresented populations.
To cite this abstract in AMA style:
Frey S, Ishaque T, Qin C, Cameron A, Massie A, Segev D, King E. Racial/Ethnic Disparities in Rates of Living Donor Liver Transplant Are Partly Explained by Socioeconomic Deprivation in Adults [abstract]. Am J Transplant. 2022; 22 (suppl 3). https://atcmeetingabstracts.com/abstract/racial-ethnic-disparities-in-rates-of-living-donor-liver-transplant-are-partly-explained-by-socioeconomic-deprivation-in-adults/. Accessed February 16, 2026.« Back to 2022 American Transplant Congress