Race Inequity in Liver Transplant Waitlisting: Effect Modification by Psychosocial Factors and the Stanford Integrated Psychosocial Assessment for Transplant
S. Deutsch-Link1, L. Nephew2, E. Weinberg3, R. Weinrieb4, M. Serper3
1Gastroenterology & Hepatology, University of North Carolina, Chapel Hill, NC, 2Gastroenterology & Hepatology, Indiana University, Chapel Hill, NC, 3Gastroenterology & Hepatology, University of Pennsylvania, Philadelphia, PA, 4Psychiatry, University of Pennsylvania, Philadelphia, PA
Meeting: 2022 American Transplant Congress
Abstract number: 75
Keywords: Liver failure, Liver transplantation, Psychosocial, Waiting lists
Topic: Clinical Science » Organ Inclusive » 70 - Non-Organ Specific: Disparities to Outcome and Access to Healthcare
Session Information
Session Name: Disparities to Outcome and Access to Healthcare
Session Type: Rapid Fire Oral Abstract
Date: Sunday, June 5, 2022
Session Time: 3:30pm-5:00pm
 Presentation Time: 4:40pm-4:50pm
Presentation Time: 4:40pm-4:50pm
Location: Hynes Room 311
*Purpose: Race inequity in liver transplantation (LT) has been a longstanding area of injustice within the field of hepatology. Information from psychosocial evaluations and The Stanford Integrated Psychosocial Assessment for Transplant (SIPAT) may provide insight into underlying processes that drive racial inequities in LT access and outcomes. Our study’s aims were to: 1) examine racial and ethnic differences in transplant waitlisting, and 2) investigate how psychosocial factors, the SIPAT score, and specific SIPAT domain scores explain the relationship between race/ethnicity and transplant waitlisting.
*Methods: We conducted a retrospective study of 1,357 patients evaluated for LT between 2014 and 2018. A multivariable logistic regression adjusting for education, insurance status, age, gender, and SIPAT domain scores assessed the relationship between race/ethnicity and transplant waitlisting. The Cochran-Mantel-Haenszel method was used to assess effect measure modification.
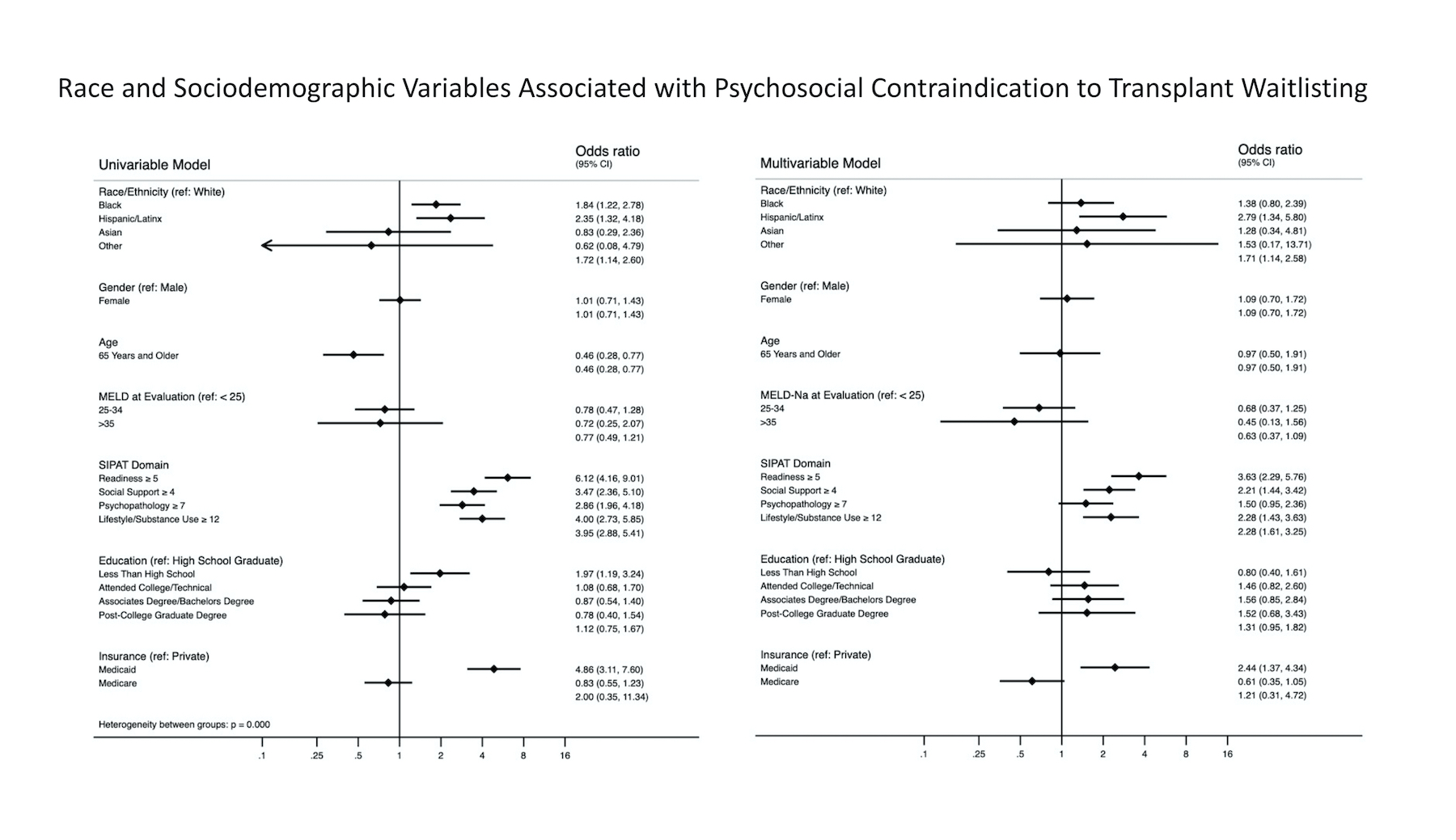
*Results: 707 patients (52%) were waitlisted for LT. On univariable analysis, Black (OR 1.84 95% CI 1.22-2.78) and Hispanic/Latinx (OR 2.35 95% CI. 1.32-4.18) patients were more likely to be declined for waitlisting due to psychosocial contraindications. After adjusting for psychosocial factors in a multivariable model, these relationships were attenuated – Black (OR 1.38 95% CI 0.80-2.39) and Hispanic/Latinx (OR 2.07 95% CI. 1.34-5.60). (Figure 1) The Cochran-Mantel-Haenszel method to determine effect measure modification demonstrated that Medicaid insurance, less than a high school education, total SIPAT score, and each of the SIPAT domains (Readiness, Social Support, Psychopathology and Lifestyle/Health Behaviors) were significant effect modifiers of the relationship between race and being declined for transplant waitlisting due to psychosocial reasons.
*Conclusions: Black and Hispanic/Latinx patients were more likely to be declined for transplant waitlisting due to psychosocial reasons. Several psychosocial factors appear to modify the relationship between race/ethnicity and psychosocial contraindication to LT waitlisting.
To cite this abstract in AMA style:
Deutsch-Link S, Nephew L, Weinberg E, Weinrieb R, Serper M. Race Inequity in Liver Transplant Waitlisting: Effect Modification by Psychosocial Factors and the Stanford Integrated Psychosocial Assessment for Transplant [abstract]. Am J Transplant. 2022; 22 (suppl 3). https://atcmeetingabstracts.com/abstract/race-inequity-in-liver-transplant-waitlisting-effect-modification-by-psychosocial-factors-and-the-stanford-integrated-psychosocial-assessment-for-transplant/. Accessed March 7, 2026.« Back to 2022 American Transplant Congress