Proximal Splenic Artery Embolization Is A Safe And Effective Tool To Treat Two Sides Of The Same Coin After Liver Transplant: Persistent High Hepatic Artery Resistive Index And Refractory Ascites And Hydrothorax Due To Portal Hyperperfusion
Cleveland Clinic, Cleveland, OH
Meeting: 2019 American Transplant Congress
Abstract number: B324
Keywords: Hemodynamics, Post-operative complications, Ultrasonography
Session Information
Session Name: Poster Session B: Liver Retransplantation and Other Complications
Session Type: Poster Session
Date: Sunday, June 2, 2019
Session Time: 6:00pm-7:00pm
 Presentation Time: 6:00pm-7:00pm
Presentation Time: 6:00pm-7:00pm
Location: Hall C & D
*Purpose: Portal hyperperfusion(PHP) is a polymorphic and dangerous condition in liver transplant(LT) recipients.The aim of the present study was to assess the safety and the efficacy of proximal splenic artery embolization(SAE) as the treatment of choice for high hepatic artery resistive index(HA RI), refractory ascites(RA) and/or refractory hydrothorax(RH), all representing clinical manifestations of PHP.
*Methods: We conducted a retrospective analysis of all patients who underwent SAE for PHP between 2007 and 2017 at our center. Qualitative data were described using number and percent. Quantitative data were described using mean and standard deviation. Continuous variables were compared by unpaired t test and categorical variables were compared by chi square test.
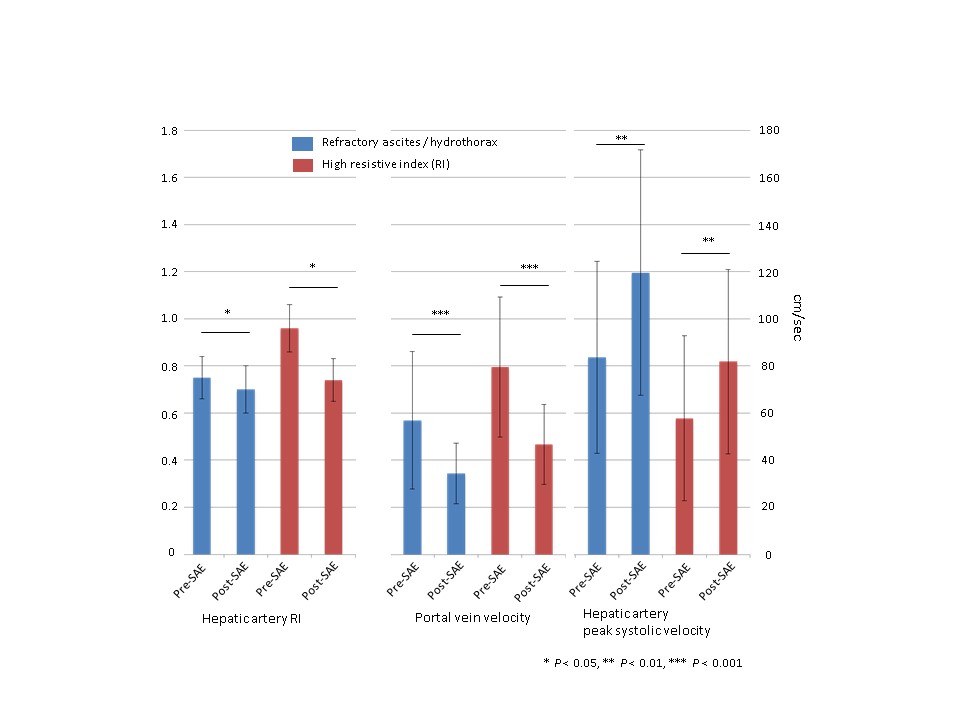
*Results: Ninety-seven patients developed PHP after LT between 2007 and 2017 and underwent SAE. The indication for SAE was elevated HA RI for 63 patients (65%) and RA and/or RH for the remaining 34 patients (35%). No significant differences were observed between the 2 groups in terms of demographic and peri-operative characteristics, with the exception for the presence of ascites in the pre transplant period in 94% of patients who later developed RA/RH against 78% of the high HA RI group (p-value = 0.04). The mean interval of follow-up after SAE was 71 ± 41 months. Normalization of liver vascular ultrasound parameters was achieved in all cases after SAE, with significant decrease of HA RI and PV velocity and concomitant increase of HA peak systolic velocity(PSV) (figure 1). The time interval between LT and SAE was 3(0-12) days in the high HA RI group and 38(7-1675) days in the RA/RH group. The median time between SAE and resolution of clinical manifestation of PHP was 1(0-13) days in the HA RI group and 34(3-762) days in the RA/RH group. Overall, the procedure was very well tolerated, with minimal incidence of post splenectomy syndrome (3 cases, 3%). Partial and subclinical splenic infarcts were incidentally discovered in 24 patients (24.7%). No cases of splenic abscess or systemic sepsis related to possible hyposplenism occurred.
*Conclusions: To our knowledge, this is the largest case series proving the safety and the effectiveness of SAE in reversing PHP and normalizing intrahepatic hemodynamics after LT. However, the clinical impact of this procedure (i.e. reduction of vascular and biliary complications) will need to be further investigated in future studies.
To cite this abstract in AMA style:
Lomaglio L, Matsushima H, Simioni A, D'Amico G, Uso TDiago, Hashimoto K, Eghtesad B, Fujiki M, Aucejo F, Sasaki K, Kwon C, Coppa C, Molano MBayona, Miller C, Quintini C. Proximal Splenic Artery Embolization Is A Safe And Effective Tool To Treat Two Sides Of The Same Coin After Liver Transplant: Persistent High Hepatic Artery Resistive Index And Refractory Ascites And Hydrothorax Due To Portal Hyperperfusion [abstract]. Am J Transplant. 2019; 19 (suppl 3). https://atcmeetingabstracts.com/abstract/proximal-splenic-artery-embolization-is-a-safe-and-effective-tool-to-treat-two-sides-of-the-same-coin-after-liver-transplant-persistent-high-hepatic-artery-resistive-index-and-refractory-ascites-and/. Accessed March 3, 2026.« Back to 2019 American Transplant Congress