Presentation and Outcomes of Post-Transplant Proliferative Disorder at a Single Institution Pediatric Transplant Center
G. Ramos-Gonzalez,1 A. Allain,1 T. Agur,1 L. O'Melia,1 S. Staffa,2 S. Burchett,1 B. Siegele,3 O. Weinberg,3 N. Rodig,1 R. Fawaz,1 T. Singh,1 D. Freiberger,1 K. Heung Bae.1
1Pediatric Transplant Center, Boston Children's Hospital, Boston, MA
2Department of Surgery, Boston Children's Hospital, Boston, MA
3Department of Pathology, Boston Children's Hospital, Boston, MA.
Meeting: 2018 American Transplant Congress
Abstract number: B360
Keywords: Epstein-Barr virus (EBV), Post-transplant lymphoproliferative disorder (PTLD), Survival
Session Information
Session Name: Poster Session B: PTLD/Malignancies: All Topics
Session Type: Poster Session
Date: Sunday, June 3, 2018
Session Time: 6:00pm-7:00pm
 Presentation Time: 6:00pm-7:00pm
Presentation Time: 6:00pm-7:00pm
Location: Hall 4EF
Purpose: The aim of this study was to characterize features present at the time of post-transplant lymphoproliferative disorder (PTLD) diagnosis, as well as outcomes, following pediatric solid organ transplantation.
Methods: We performed a retrospective review of transplant patients at our center from January 2006 to August 2016 with a diagnosis of pathologically confirmed PTLD.
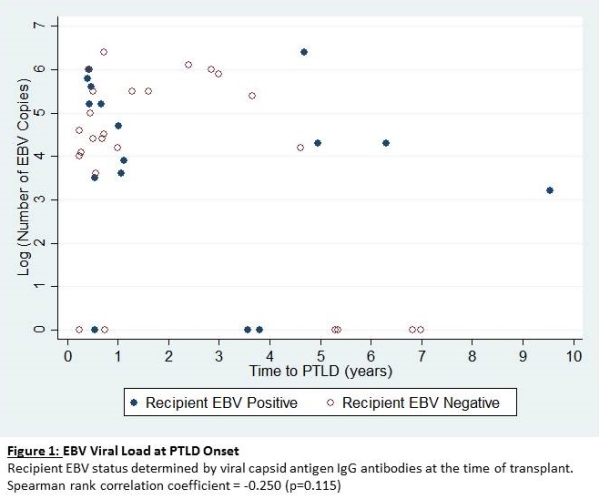
Results: Of 594 patients included in this study, 41(6.9%) were diagnosed with PTLD, 28 of whom were male. Median age at transplant was 5.6 years (IQR 1.7-16.1). Proportion of PTLD cases by organ transplanted and median time (IQR) to disease onset were: heart 11/144(7.6%) at 13.6(8.5-55.6) mo, lung 7/52(13.5%) at 9.1(4.9-35) mo, kidney 8/255(3.1%) at 39.5(13.9-57.1) mo, liver 12/125(9.6%) at 7.7(5.5-22) mo, intestine 0/4(0%) and multi-visceral 3/14(21.4%) at 5.4(5.4-5.6) mo. Liver and multi-visceral transplants had a higher propensity to develop PTLD within the first year (p<0.001 & p=0.004, respectively). EBV status and timing of development of PTLD are shown in Figure 1. There were 6 early lesions, 15 polymorphic, 19 monomorphic, and 1 uncharacterizable PTLD. Following immunosuppression reduction, 30 patients received rituximab, and 14 required chemotherapy. At median 25(IQR 12-53) months follow-up from the onset of PTLD, 8 patients died secondary to transplant related complications, 3 are alive with active disease, and 30 have no evidence of disease.
Conclusion: PTLD is a significant complication following pediatric solid organ transplantation. EBV monitoring following transplant may assist in the early detection of PTLD. The majority of patients can achieve long-term disease free survival through immunosuppression reduction with the addition of Rituximab and chemotherapy in refractory cases.
CITATION INFORMATION: Ramos-Gonzalez G., Allain A., Agur T., O'Melia L., Staffa S., Burchett S., Siegele B., Weinberg O., Rodig N., Fawaz R., Singh T., Freiberger D., Heung Bae K. Presentation and Outcomes of Post-Transplant Proliferative Disorder at a Single Institution Pediatric Transplant Center Am J Transplant. 2017;17 (suppl 3).
To cite this abstract in AMA style:
Ramos-Gonzalez G, Allain A, Agur T, O'Melia L, Staffa S, Burchett S, Siegele B, Weinberg O, Rodig N, Fawaz R, Singh T, Freiberger D, Bae KHeung. Presentation and Outcomes of Post-Transplant Proliferative Disorder at a Single Institution Pediatric Transplant Center [abstract]. https://atcmeetingabstracts.com/abstract/presentation-and-outcomes-of-post-transplant-proliferative-disorder-at-a-single-institution-pediatric-transplant-center/. Accessed February 18, 2026.« Back to 2018 American Transplant Congress