Preformed Anti-HLA Donor-Specific Antibodies Immunological Risk Assessment: The Importance of HLA Antibody Locus-Specificity
1Terasaki Research Institute, Los Angeles, CA, 2University Hospitals Coventry and Warwickshire, Coventry, United Kingdom, 3NHS Blood and Transplant, Birmingham, United Kingdom, 4University Hospitals Coventry and Warwickshire NHS Trust, Coventry, United Kingdom, 5University of Warwick Medical School, Coventry, United Kingdom
Meeting: 2020 American Transplant Congress
Abstract number: A-011
Keywords: Highly-sensitized, HLA antibodies, Kidney transplantation
Session Information
Session Name: Poster Session A: Kidney Acute Antibody Mediated Rejection
Session Type: Poster Session
Date: Saturday, May 30, 2020
Session Time: 3:15pm-4:00pm
 Presentation Time: 3:30pm-4:00pm
Presentation Time: 3:30pm-4:00pm
Location: Virtual
*Purpose: The screening of preformed donor-specific HLA antibodies (pfDSA) by single antigen bead assays has increased the complexity of pre-transplant patient risk stratification. We evaluated the different characteristics of pfDSA that may confer a risk for early rejection episodes.
*Methods: We retrospectively studied 97 HLA sensitized kidney recipients transplanted between 2004 and 2015 at the University Hospitals Coventry and Warwickshire, UK. All recipients received Basiliximab induction immunosuppression therapy. The absolute proportions of HLA sensitized recipients that experienced an early rejection episode by day 98 post-transplantation were assessed using univariate and multivariate Cox proportional hazards models.
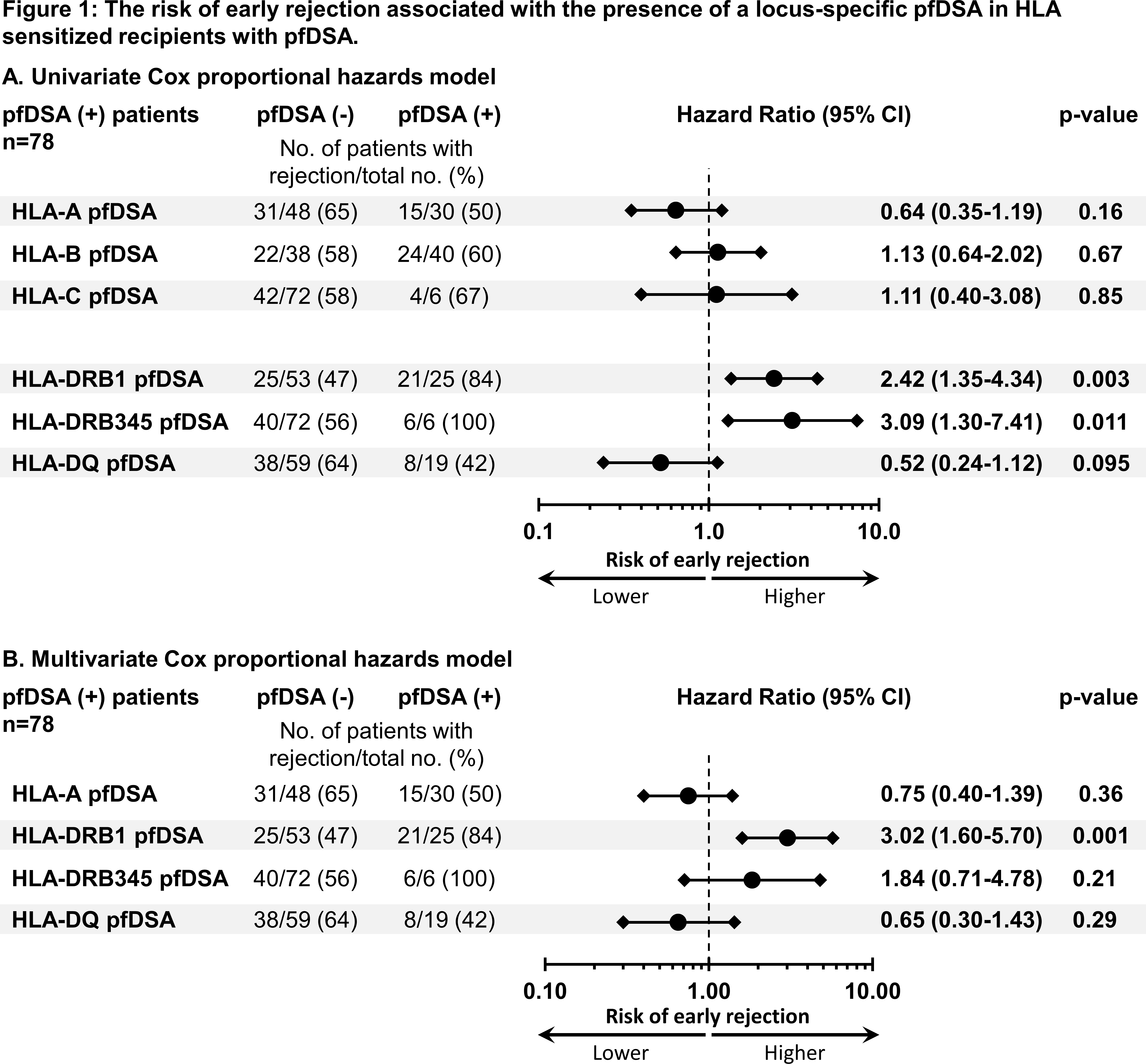
*Results: Among the 97 HLA sensitized recipients, 51% experienced an early rejection episode, and 80% were transplanted in the presence of at least one pfDSA and 20% were transplanted in the presence of preformed non-DSA. The presence of at least one pfDSA was associated with an increased risk for an early rejection episode as compared to not having a pfDSA (HR (95% CI)=5.02 (1.56-16.17), p=0.007). Among the 78 pfDSA positive recipient, there was no significant difference in the cumulative event rate of early rejection between HLA class specificities, number of pfDSA, and pfDSA MFI strength. The univariate analysis revealed that the presence of a pfDSA directed against HLA-DRB1 or -DRB345 was associated with a significantly increased risk for an early rejection episode as compared to having a pfDSA against other HLA loci (HR (95% CI)=2.42 (1.35-4.34), p=0.003, and HR (95% CI)=3.09 (1.30-7.41), p=0.011, respectively). The multivariate model revealed that only the presence of pfDSA directed against HLA-DRB1 was associated with a significantly increased risk for an early rejection episode (HR (95% CI)=3.02 (1.60-5.70), p=0.001) (Figure 1).
*Conclusions: This study demonstrated that, under Basiliximab induction therapy, pfDSAs directed against HLA-DRB1 had the highest pathogenic potential towards early acute rejection episodes as compared to pfDSAs directed against other HLA loci. The result of this study suggests that certain pfDSA should be taken into account in pre-transplant risk assessment.
To cite this abstract in AMA style:
Jucaud V, Babu A, Briggs D, Krishnan N, Mitchell D, Everly M. Preformed Anti-HLA Donor-Specific Antibodies Immunological Risk Assessment: The Importance of HLA Antibody Locus-Specificity [abstract]. Am J Transplant. 2020; 20 (suppl 3). https://atcmeetingabstracts.com/abstract/preformed-anti-hla-donor-specific-antibodies-immunological-risk-assessment-the-importance-of-hla-antibody-locus-specificity/. Accessed March 4, 2026.« Back to 2020 American Transplant Congress